AJH:单剂量与低剂量利妥昔单抗治疗皮质类固醇耐药或复发性 ITP:一项多中心、随机、对照研究
2022-02-08 MedSci原创 MedSci原创
这项研究结果表明,单次输注375mg/m2的RTX是安全有效的,与治疗皮质类固醇耐药或复发的ITP的低剂量RTX的疗效相似
原发性免疫性血小板减少症(ITP)是一种自身免疫性出血疾病,在推荐的二线治疗中,利妥昔单抗(RTX)诱导了最佳的长期效果。然而,利妥昔单抗的最佳治疗方案仍不清楚。在此研究人员开展了一项前瞻性、多中心、开放标签、随机对照试验,以比较 RTX 在两种不同剂量方案中对皮质类固醇耐药或复发性 ITP 患者的疗效和安全性。
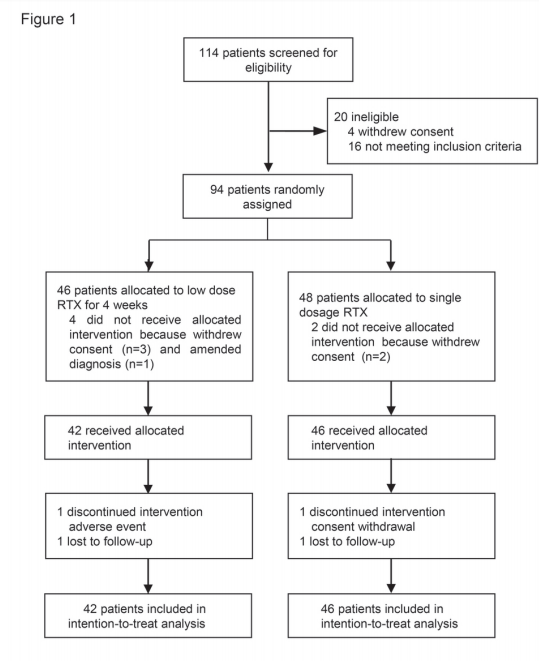
图1:研究设计和处理处置。
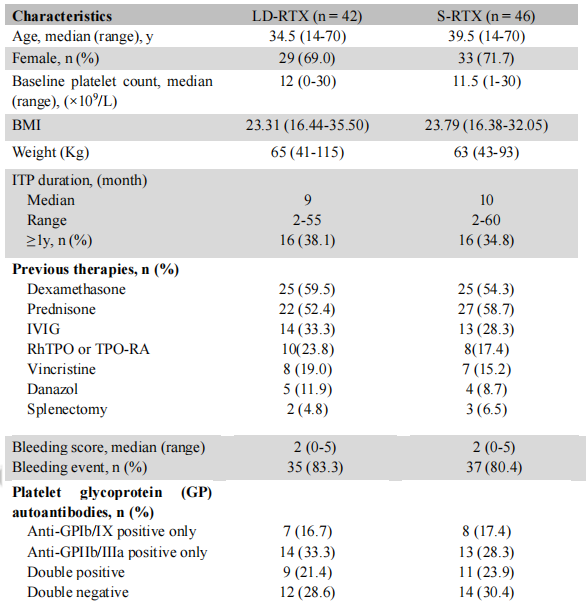
表1:患者的人口统计学特征和基线特征。除非另有说明,否则数据均为n(%)或中位数(范围)。体重指数(BMI)是指体重(kg)除以身高的平方(m)。IVIG,静脉注射免疫球蛋白。rhTPO,重组人血小板生成素;TPO,血小板生成素。缩写:GPIb/IX、血小板糖蛋白Ib/IX;GPIIb/IIIa、血小板糖蛋白IIb/IIIa;
研究团队招募的患者被随机分配 (1:1) 接受重复低剂量 RTX(每周 100 mg,持续 4 周,LD-RTX)或单剂量(375 mg/m2,S-RTX)。接受 LD-RTX 的患者与接受 S-RTX 的患者分别有 64.3%和 67.4% 的总体反应(p =0.759)。LD-RTX 后的完全缓解 (CR) 率为 23.8%,S-RTX 后为 28.3% (p = 0.635)。
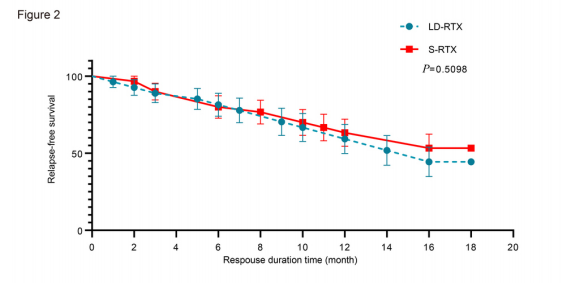
图2:初始反应患者(包括CR和R)的Kaplan-Meier反应持续时间曲线。Kaplan-Meier曲线显示,在整个随访期间,两组患者的总体反应持续时间相似。(P = 0.5098)
在与健康相关的生活质量方面,与 LD-RTX 相比,S-RTX 改善了患者的心理状态、生活质量、社会活动和工作。此外,S-RTX 在不影响疗效的情况下显着减少了就诊次数。
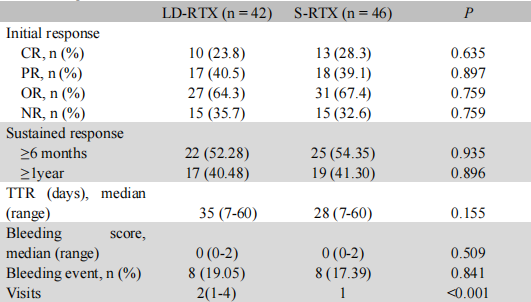
表2:LD-RTX组和S-RTX组的反应和结果。数据以n(%)名患者表示。
总之,这项研究结果表明,单次输注375mg/m2的RTX是安全有效的,与治疗皮质类固醇耐药或复发的ITP的低剂量RTX的疗效相似。常见的临床益处包括改善与健康相关的生活质量和减少医生就诊次数。对于类固醇耐药或复发的ITP,单剂量的标准RTX比低剂量的-RTX是一种很有前途和更方便的治疗方法。
原始出处:
, , , et al. Single-dose versus low-dose rituximab in corticosteroid-resistant or relapsed ITP: A multicenter, randomized, controlled study. Am J Hematol. 2022; 1- 8. doi:10.1002/ajh.26473
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#多中心#
56
#利妥昔#
52
#对照#
41
#复发性#
34
#类固醇#
37
#ITP#
0
#低剂量#
39