Blood:HLA-B先导基因型预测HLA错配无血缘关系供体HCT的预后
2020-06-07 QQY MedSci原创
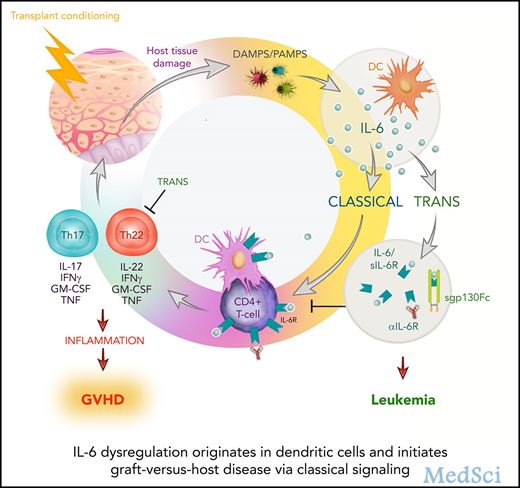
来自HLA不匹配的无血缘关系的捐赠者的造血细胞移植(HCT)可以治愈危及生命的血液疾病,但其成功率受到移植物抗宿主病(GVHD)的限制。HLA-B先导基因在第2号位置上编码蛋氨酸(M)或苏氨酸(T),
Petersdorf等人确定了1988年-2016年期间从HLA-A、-B、-C、-DRB1或-DQB1不匹配的无血缘捐赠者那里移植的11872例患者的先导基因型。采用多变量回归方法,根据HLA基因座不匹配评估与患者先导基因型相关的风险因素;根据和患者先导基因型评估与HLA- A、-B、-C、-DRB1或-DQB1不匹配相关的风险。
患者先导基因型对急性GVHD和死亡率的影响因HLA基因座的不同而不同。与HLA-DQB1错配的TT型患者相比,HLA-DQB1错配的MM患者的非复发死亡率更高(风险比 1.35,p=0.01)。与HLA-DRB1错配的TT型患者相比,HLA-DRB1错配的MM型或MT型患者的III-IV级GVHD风险更高(优势比分别是2.52和1.51)。
患者对HLA-DQB1单位点错配的耐受性优于其他位点的错配。HLA-不匹配移植后的预后取决于HLA-B先导的二态性和HLA基因座不匹配。
综上所述,患者先导基因变异为HLA错配的限制提高了新的信息。或可根据患者先导基因来明智的选择不匹配的捐赠者来提高HLA不匹配的无血缘关系的移植的成功率。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#基因型#
39
#供体#
47
#HLA-B#
52
#HCT#
0
#HLA#
32