PNAS:美研究人员研制出新型血检,可快速诊断结核病仅需两个半小时
2017-03-28 新华社 林小春
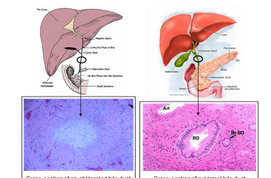
美国研究人员3月27日在美国《国家科学院学报》上报告说,他们研制出一种新型血液检测方法,仅需两个半小时就能诊断结核病,并快速判断病人的治疗情况。这项成果可能有助改善结核病诊断方法。据世界卫生组织估计,全球每年有约1000万人患结核病,约200万人因结核病死亡,其中许多人死亡的原因是未得到诊断或确诊太晚以致无法治愈。全球有三分之一的人感染结核杆菌却并不发病,其中约10%的人最终会患上结核病。因此,研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PNAS#
37
#研究人员#
25
#半小时#
22
#结核#
28
#血检#
35