头痛是一种难以处理的常见病,严重影响患者健康,并且造成了巨大的社会负担。近期,英国国家医疗卫生与临床优选研究所(NICE)对《12岁及以上头痛的诊断和治疗指南》(2012年版)进行了更新,以及为常见头痛的诊治以及因药物过度使用所致的头痛的预防提供一些简明的建议,具体如下:
一、头痛的诊断

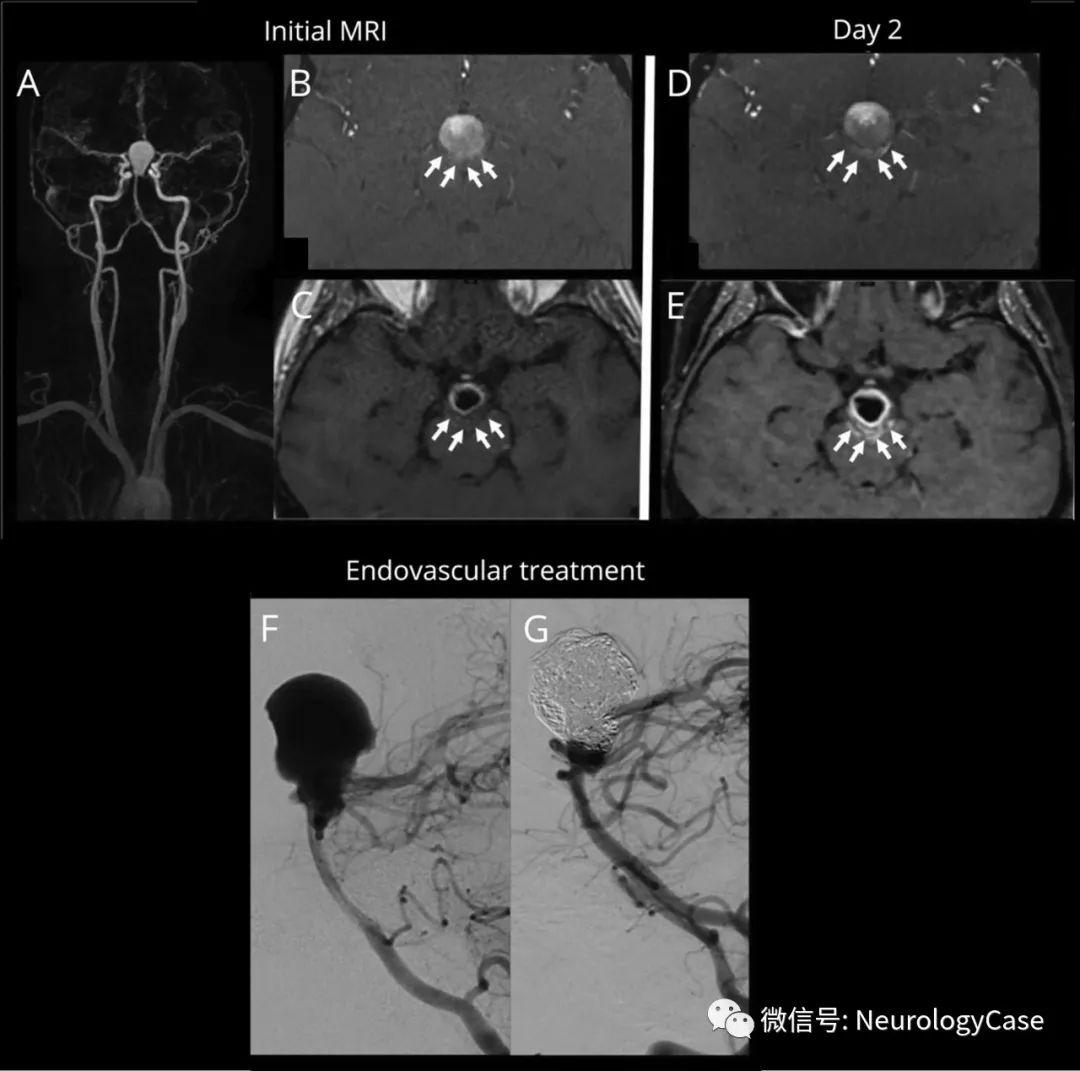
图1 紧张型头痛、偏头痛、丛集性头痛的诊断
月经相关性偏头痛:在三个连续月经周期中(至少有两个周期),在月经前2天至月经后3天,女性出现可疑月经相关偏头痛。
药物过度使用头痛:如患者在服用以下药物3个月或以上期间出现头痛或加重,请留意药物过度使用的可能性:
-
每月10天或以上服用曲坦类药物、阿片类药物、麦角类药物或联合镇痛药物;
-
乙酰氨基酚、阿司匹林或非甾体抗炎药(非甾体抗炎药或非甾体抗炎药),可单独服用或任意组合服用,每月服用15天或更长时间。
-
应用阿司匹林、乙酰氨基酚或非甾体抗炎药治疗时要考虑患者的个人情况、并发症和不良事件的风险。鉴于与瑞氏综合征(一种以急性脑病合并肝功能损害为特征的临床综合征)有关,不建议16岁以下的患者使用含阿司匹林的制剂;
-
不建议使用阿片类药物。
-
可考虑5~8周共10个疗程的针灸用于预防治疗慢性紧张型头痛。
2.偏头痛(有或无先兆)
-
采用口服曲坦和非甾体抗炎药或口服曲坦和乙酰氨基酚的联合应用治疗,应考虑患者的个人情况、并发症和不良事件的风险。12~17岁的患者,优先考虑经鼻用的曲坦类制剂,而不是口服曲坦类制剂。
-
对于倾向于只服用一种药物的患者,可以考虑口服曲坦、非甾体抗炎药、阿司匹林或乙酰氨基酚。
-
在偏头痛的其他急性治疗中,即使没有恶心和呕吐,也可以考虑使用止吐剂。
-
不建议麦角或阿片类药物。
-
对于口服制剂(或12至17岁年轻人的鼻用制剂)在偏头痛急性治疗中无效或不耐受的人:考虑胃复安或丙氯拉嗪的非口服制剂;如果以前没试过非口服非甾体抗炎药或曲坦类患者,也可考虑加用。
-
注意胃复安和丙氯拉嗪产品说明书中的特别警告和注意事项,并与患者(或其父母或照护者,视情况而定)讨论其益处和风险。
-
根据患者个人情况、共病、不良事件的风险的差异及头痛对生活质量的影响,可以考虑提供托吡酯或普萘洛尔,但托吡酯可引起胎儿畸形的风险增加、降低激素类避孕药的疗效。因此,有生育能力的妇女和女孩,若服用托吡酯治疗,要确保提供合适的避孕措施(例如,使用醋酸甲羟孕酮储备注射剂、宫内避孕法或激素避孕结合屏障法)。
-
抑郁症和偏头痛共病的患者使用普萘洛尔可能会增加自残的风险,因此,开普萘洛尔处方时要谨慎。
-
根据患者个人情况、并发症和不良事件的风险,可考虑使用阿米替林。
-
不建议使用加巴喷丁。
-
如果托吡酯和普萘洛尔都不适合或者无效,根据患者个人情况、并发症和不良事件风险的差异,可考虑在5~8周内进行最多10个疗程的针灸治疗。
-
对于已经在接受另一种预防疗法的患者,其偏头痛得到了很好的控制,可根据需要继续目前的治疗。
-
在预防性治疗6个月后,需评估继续进行偏头痛预防的必要性。
-
对有些偏头痛的患者,建议服用核黄素(400 mg,每天一次)可减少偏头痛的频率和强度。
-
对于有先兆偏头痛的患者,常规不应提供复合激素类避孕药来避孕。
-
对于可预见偏头痛与月经有关、且对标准的急性期治疗效果不好的女性,预计在偏头痛发作的日子,可考虑给予夫罗曲坦(2.5 mg,2次/天)或佐米曲坦(每次2.5 mg,2~3次/天)。
-
在考虑了妇女的治疗需求和怀孕期间使用每种药物的相关风险后,可使用曲坦或非甾体抗炎药。如果怀孕期间需要对偏头痛进行预防性治疗,建议咨询专家。
-
可给氧气、皮下或经鼻曲坦治疗
-
当急性期治疗用氧气时:使用100%氧气,可用戴上非循环式面罩和储氧袋,氧气流速至少12升/分钟;安排提供家庭临时性及便携式氧气。
-
在经皮下或经鼻使用曲坦药物时,应确保为患者提供足够的曲坦类药物。这应该根据患者以往丛集性头痛发作的次数来计算,还应考虑药物每日的最大每日剂量。
-
不推荐使用乙酰氨基酚,非甾体抗炎药,阿片类药物,麦角或口服曲坦类药物。
-
考虑使用维拉帕米作预防性治疗丛集性头痛时,如果不熟悉其使用情况,在使用维拉帕米前,应咨询专家意见,包括必要时进行心电图监测。
-
若维拉帕米治疗集束性头痛无效,应寻求专家建议。
-
若怀孕期间需要治疗丛集性头痛,应寻求专家建议。
-
向服用过量药物引起头痛的患者解释,可以通过停用过度使用的药物来治疗头 痛。
-
建议患者停止服用过度治疗急性头痛的药物至少1个月,应突然停用,而不是逐渐停用。
-
要提醒患者:停用过度使用的药物,头痛症状在改善之前,短时间内可加重甚至伴有阶段症状。要密切随访,根据患者的需要提供帮助。
-
对潜在原发性头痛,除了要停用过度使用的药物,还应考虑预防性治疗。
-
不要经常为过度使用药物引起的头痛提供住院停药。
-
对于正在使用强剂量阿片类药物、或有相关并发症、或先前多次尝试停用过度使用药物失败的患者,可以考虑专科转诊和/或住院患者停用过度药物。
-
在停用过度使用的药物后4~8周,复查过度用药性头痛的诊断和进行进一步的管理。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
41
学习
49
#NICE#
46
#诊治指南#
40
#学习#
64
好好学习
45
只要主义真学习学习学习学习学习学习学习学习学习学习学习学习学习学习
60