Investigative Radiology:如何利用先进的影像技术提高床旁胸部x线片的图像质量?
2022-09-09 shaosai MedSci原创
为了提高没有物理网格(无网格)的放射线照片的图像质量(IQ),Fujifilm公司(日本东京)开发了软件(SW),商业上称为虚拟网格。
众所周知,重症监护室(ICU)每天都要进行床边胸部X射线检查以实现对呼吸系统或心血管疾病患者的病程进行评估。现阶段,在床边检查中使用物理网格并不常见,因为当X射线焦点没有正确地对准物理网格时,射线照片中会出现错位伪影。
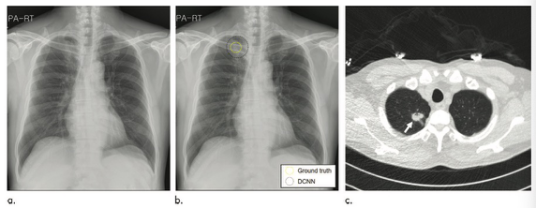
为了提高没有物理网格(无网格)的放射线照片的图像质量(IQ),Fujifilm公司(日本东京)开发了软件(SW),商业上称为虚拟网格。最近的一篇文章讨论了虚拟网格软件在对比度细节模型-CDRAD 2.0上的应用,显示了其改善图像方面的价值。然而,这项研究只评估了应用于技术模型x线照片的虚拟网格的性能。因此,有必要对使用和不使用虚拟网格处理的临床病人胸部X光片进行评估。
近日,发表在Investigative Radiology杂志的一项研究评估了虚拟网格在临床ICU胸片上的表现,为提高图像质量、提高医生的诊断信心提供可技术支持。

图 A-E,分别是气管、肋骨、肺、脊柱和心脏后面的肺的一部分选定区域。从左到右,感兴趣的区域分别用虚拟网格SW比0(SC SW关闭)、6:1(R6)、10:1(R10)、13:1(R13)、17:1(R17)和20:1(R20)处理
本研究表明,当虚拟网格与SW网格比为6:1时可显著提高无网格胸部床旁x线片的图像质量。同时发现,应慎重考虑使用17:1和20:1的网格比,因为SW对部分肋骨和脊柱会产生不利影响,建议将网格比率提高到13:1以解决相关问题。
原文出处:
Tim Gossye,Dimitri Buytaert,Peter V Smeets,et al.Evaluation of Virtual Grid Processed Clinical Chest Radiographs.DOI:10.1097/RLI.0000000000000876
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
33
#X线#
45
#X线片#
38
#IgA#
40