Am J Resp Crit Care:血小板调节肺结核的炎症和组织破坏!
2018-02-09 xing.T MedSci原创
由此可见,血小板促进TB患者炎症和组织降解。
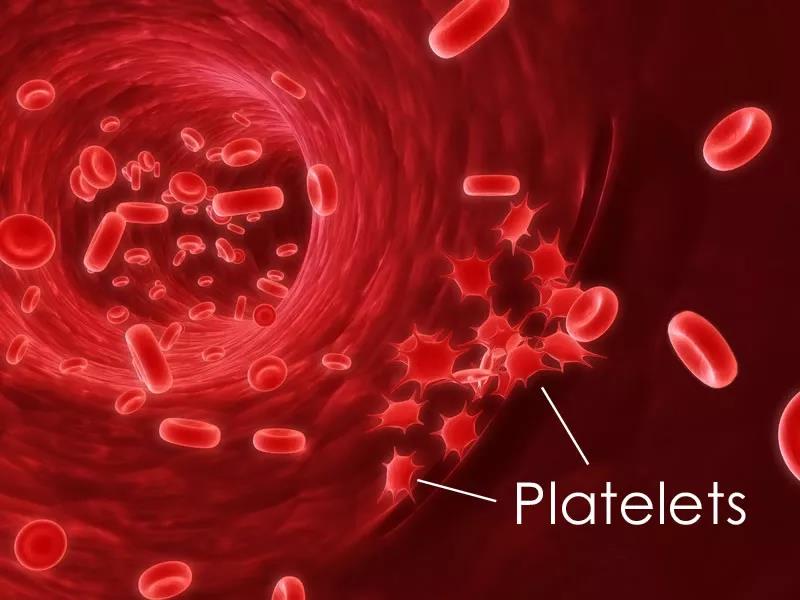
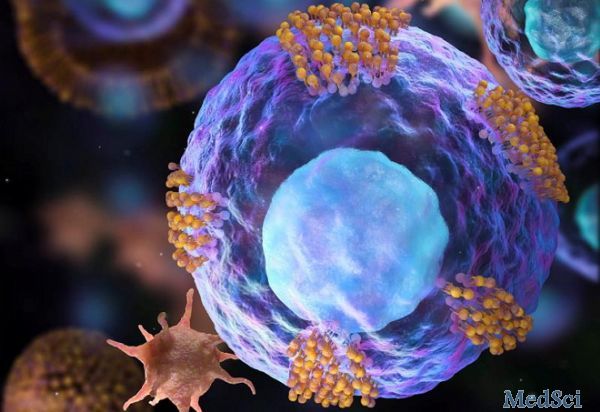
结核病(TB)患者的血小板可能与免疫系统相互作用,以调节导致感染发病和传播的人类炎症反应。近日,呼吸内科以及重症医学领域权威杂志Am J Resp Crit Care上发表了一篇研究文章,该研究旨在明确血小板在TB患者先天性炎症和基质降解反应中的功能作用。
研究人员对50名治疗前的TB患者和50名对照者血浆中的血小板活化标志物进行了检测,并纵向随访了25例患者。在感染活的强毒结核分枝杆菌(M.tb)的共培养模型中研究血小板-单核细胞相互作用,并使用Qpcr、Luminex多重阵列、基质降解测定和菌落计数进行分析。免疫组织化学检测肺TB小鼠模型的CD41表达,并对来自于15名TB患者和匹配的对照者支气管肺泡灌洗液(BALF)测量分泌的血小板因子水平。
与对照组相比,TB患者六种血小板相关介质中的五种在血浆中有所上调,在治疗的第60天时浓度回到基线。在M.tb感染中,单核细胞胶原酶MMP-1的基因表达可被血小板上调。血小板还增强了M.tb诱导的MMP-1和MMP-10分泌,这导致了I型胶原降解。与M2单核细胞表型一致,血小板增加了单核细胞IL-1和IL-10,并降低了IL-12和单核细胞衍生的趋化因子(MDC,也称为CCL-22)分泌。细胞内M.tb的单核细胞杀伤作用减弱。在TB小鼠模型的肺脏中可以检测到血小板,并且在人BALF中分泌的血小板介质有所上调,并且与MMP和IL-1β浓度相关。
由此可见,血小板促进TB患者炎症和组织降解。
原始出处:
Katharine A Fox,et al. Platelets Regulate Pulmonary Inflammation and Tissue Destruction in Tuberculosis.AM J RESP CRIT CARE 2018. https://doi.org/10.1164/rccm.201710-2102OC
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#组织破坏#
43
一起学习学习
62
一起学习学习
50
一起学习学习
48
#结核#
31
一起学习学习
50
阅
42
阅
30
学习了受益匪浅
34
结核病(TB)患者的血小板可能与免疫系统相互作用.以调节导致感染发病和传播的人类炎症反应.近日.呼吸内科以及重症医学领域权威杂志AmJRespCritCare上发表了一篇研究文章.该研究旨在明确血小板在TB患者先天性炎症和基质降解反应中的功能作用.
34