IBD:接受托法替尼治疗的溃疡性结肠炎患者带状疱疹感染的长期风险变化
2022-06-04 xuyihan MedSci原创
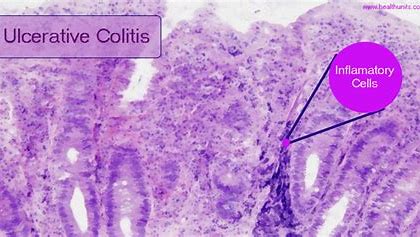
溃疡性结肠炎是一种病因尚不十分清楚的结肠和直肠慢性非特异性炎症性疾病,病变局限于大肠黏膜及黏膜下层。病变多位于乙状结肠和直肠,也可延伸至降结肠,甚至整个结肠。
溃疡性结肠炎 (UC) 是关于结肠黏膜的一种慢性炎症性疾病,可导致直肠出血、腹泻、大便紧迫和其他可能使人衰弱的肠道症状。患有 UC 和其他慢性炎症性自身免疫性疾病的患者发生各种感染的风险较高,包括由潜伏水痘带状疱疹病毒 (VZV) 重新激活引起的带状疱疹 (HZ;即带状疱疹)。
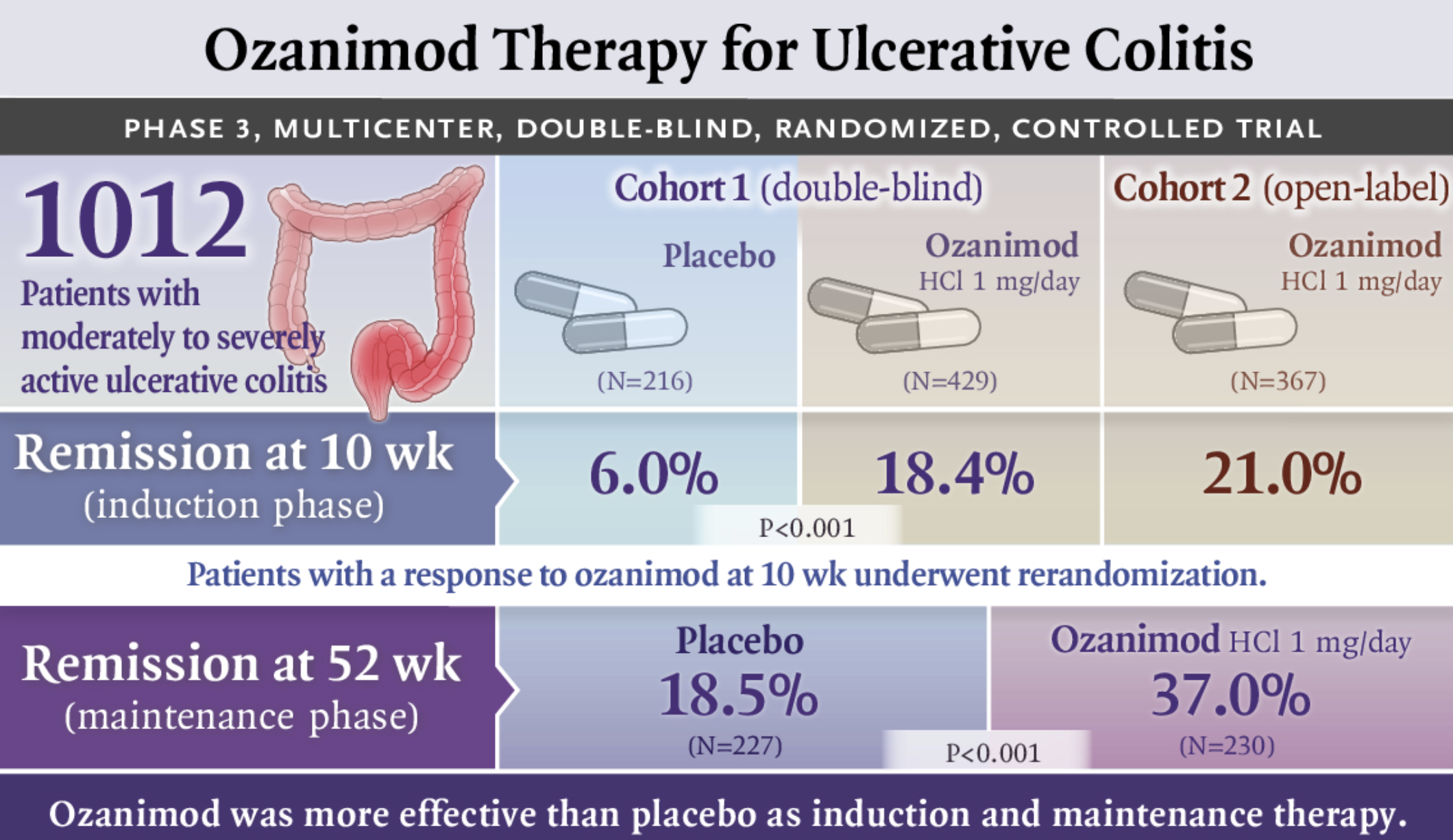
此外,在接受用于治疗 UC 的治疗(例如皮质类固醇、硫嘌呤和肿瘤坏死因子抑制剂 (TNF))的患者中,HZ 风险可能会进一步增加。托法替尼(Tofacitinib) 是一种口服小分子 Janus 激酶 (JAK) 抑制剂,用于治疗 UC。本项研究旨在探究托法替尼 治疗UC 的临床项目中(长达 7.8 年)中带状疱疹 (HZ) 的发病率和危险因素。
研究人员在4个UC队列中评估 HZ 的比例和发生率(事件发生率(IR):事件/100 患者年):诱导(第 2 期和第 3 期诱导研究数据)、维持(第 3 期维持研究数据)、总体(来自所有2、3 期和开放标签长期扩展研究),以及总体加上6个月的中期3b和4期数据。最后通过 Cox 回归分析评估带状疱疹的危险因素。

研究结果显示:在诱导和维持队列中,托法替尼 10 mg 每天两次 (BID) 与安慰剂和托法替尼10与5mg BID相比,HZ(非严重和严重)的IR在数值上更高。对于所有托法替尼剂量(5 或 10 mg BID),总体和总体加 3b/4 期队列(总暴露量分别为 2814.4 和 2999.7 患者年)中 HZ 的 IR(95% 置信区间)为 3.38(2.73- 4.15) 和 3.30 (2.67-4.04)。在整体加阶段 3b/4 队列中,>90% 的 HZ 是非严重的;>90% 为轻度/中度;>90%的患者在不停止托法替尼的情况下可以得到解决;0.6%的患者有多个 HZ 事件。带状疱疹的危险因素包括年龄较大以及体重较轻。
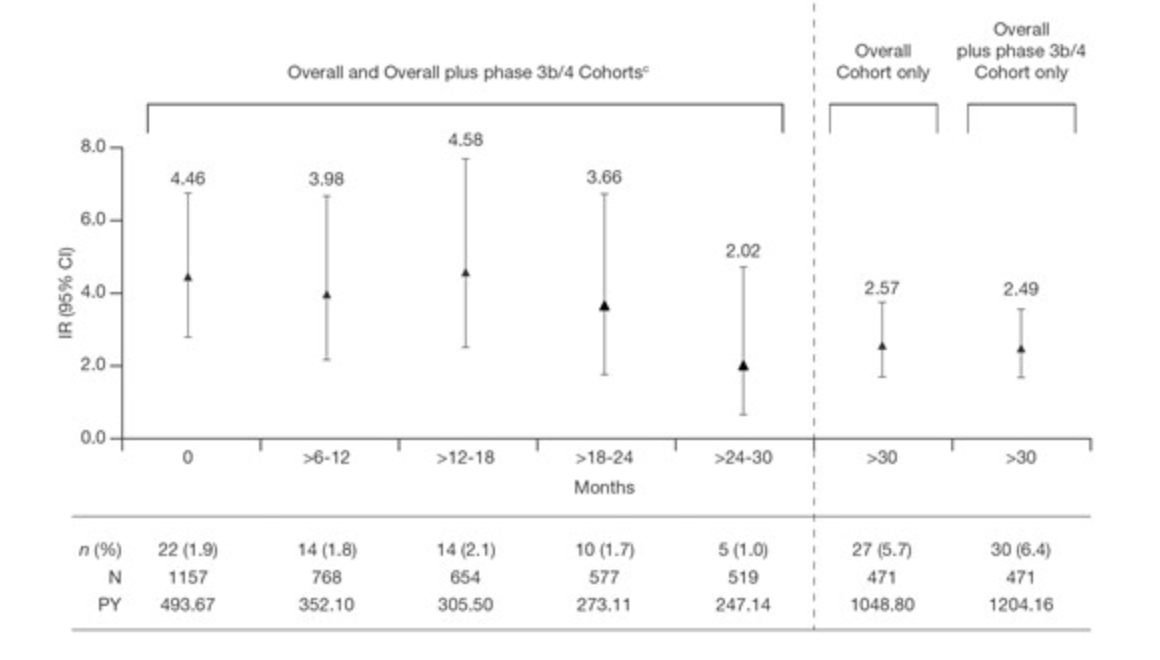
本项研究证实大多数UC患者发生HZ事件是轻度/中度的。带状疱疹IR在 7.8 年的暴露期间保持稳定。年龄较大、体重较轻和先前的TNF失败与 HZ 风险增加有关。
原始出处 :
Kevin L Winthrop. Et al. Long-term Risk of Herpes Zoster Infection in Patients With Ulcerative Colitis Receiving Tofacitinib. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#溃疡性#
42
#IBD#
40
#长期风险#
41
#疱疹#
72