Cell:重磅!利用synNotch T细胞直接运送药物到肿瘤中
2016-10-05 佚名 生物谷
在一项新的研究中,来自美国加州大学旧金山分校的研究人员构建出能够精确地确定患病细胞在体内任何位置和执行一系列可定制反应(customizable responses)的人免疫细胞,包括将药物或其他治疗运载物直接运送到肿瘤或其他不健康的组织中。在小鼠体内开展的实验中,这些被称作synNotch (synthetic Notch) T细胞的免疫细胞高效地靶向肿瘤,释放一种特定的人抗体药物,
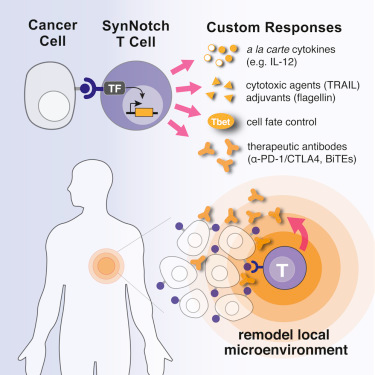
除了运送治疗性试剂外,synNotch T细胞能够经编程后以多种其他的方式杀死癌细胞。不过synNotch T细胞也能够执行抑制免疫反应的指令,从而为这些细胞能够被用来治疗1型糖尿病等自身免疫疾病或者局部抑制移植器官遭受的免疫系统排斥提供可能。
论文通信作者、加州大学旧金山分校细胞与分子药理学教授Wendell Lim博士说,“synNotch T细胞是一种通用的分子检测器,允许我们对免疫细胞进行编程就好比它们是微型机器人一样。它们能够经定制化设计后具有不同的特征和功能,而且当它们检测到患病组织中合适的信号时,它们能够经触发后部署多种治疗武器。”
绕过CAR-T细胞疗法的限制
这项新研究拓宽和加深了Lim实验室之前对synNotch T细胞的研究,其中后者已证实synNotch传感器平台能够被用来在T细胞中构建自定义的“逻辑门”,从而允许它们识别和杀死癌细胞,同时保护关系比较密切的健康细胞。这些细胞“AND门”需要在靶细胞中满足两个独立的条件,这样T细胞才会采取行动清除这些靶细胞。
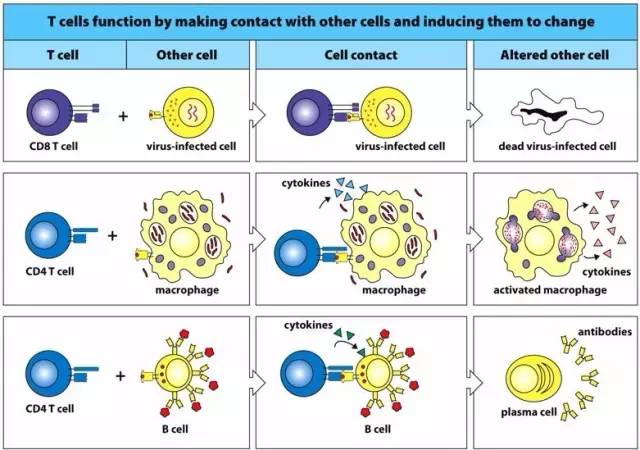
T是高度迁移性的,在全身各处移动以便寻找患病的或被感染的细胞。一种被称作嵌合抗原受体T细胞(CAR-T)疗法的T细胞疗法因其在治疗一种被称作急性淋巴细胞白血病(ALL)的血癌中取得史无前例的成功而被公之于众。
但是鉴于CAR-T细胞疗法主要依赖于T细胞“内置的”检测和反应性质,而且其中的一些性质能够是有害的,因此它能够产生严重的副作用。再者,因为T细胞经常不能够战胜肿瘤抑制免疫反应的性质,所以CAR-T细胞疗法迄今为止并不能够有效地治疗影响乳腺、前例腺、大脑、肺部和其他器官的实体瘤。Lim说,加州大学旧金山分校开发的这种synNotch技术能够独立使用,不过它也能够与CAR-T细胞一起使用以便绕过CAR-T细胞疗法当前所面临的很多限制。
synNotch之所以如此称呼是因为它是Notch蛋白的几种人工合成变化的产物,其中Notch蛋白参与许多种有机体中的细胞间通信,而且在正常发育中发挥着特别至关重要的作用。首先,synNotch受体作为一种“通用传感器”发挥作用---它拥有一种从T细胞中延伸出来的组分,而且这种组分能够发生交换从而特异性地识别很多不同类型的疾病信号。synNotch的另一端是一种“效应”组分位于T细胞内,能够经改造后导致T细胞执行各种各样的反应。
synNotch多功能性
在这项新的研究中,论文第一作者Kole T. Roybal博士等人以多种方式证实了synNotch T细胞的多功能性。
(1)当遭受激活时,包括CAR-T细胞在内的常规性T细胞分泌“天然的”一套细胞因子,即召唤其他免疫细胞到患病位点和决定整体免疫反应的化学信号。但是一些天然的细胞因子当过量产生时也能够是高度有毒性的。来自Lim实验室的一些研究人员证实synNotch T细胞能够经激活后分泌单个事先确定的细胞因子或者定制的细胞因子组合,而且这些组合能够经调整后触发所需要的特异性免疫反应。
(2)synNotch T细胞也能够携带其他受体,其中这些受体通过触发内在的细胞死亡通路导致它们靶向的患病细胞“自杀”。
(3)当T到达患病位点并且被激活时,它们可能转化为特定的T细胞亚型。当与细胞因子在一起时,因这种转化产生的T细胞亚型可能并不是最佳的组合。Lim和同事们证实当利用synNotch技术时,这种T细胞转化过程能够发生“偏斜”以至于这些被激活的T细胞经优化后产生抵抗癌症的T细胞亚型。
(4)使用所谓的启动免疫反应的“免疫检查点抑制剂”药物在治疗转移性黑色素瘤和其他直到最近还被认为是致命性的癌症中实现史无前例的病情缓解。在这项新的研究中,synNotch T细胞经改造后当与肿瘤直接接触时会产生两种有效的免疫检查点抑制剂药物。Lim说,这种靶位点药物运送可能增加癌症病人的反应,同时降低副作用。利用synNotch运送另一种被称作双特异性T细胞接合器(Bispecific T Cell Engager, BiTE)的分子可消除小鼠体内的肿瘤,同时不会影响正常的细胞。
(5)有趣的是,研究人员证实synNotch T细胞能够在患病位点产生免疫抑制性信号,这就表明synNotch T细胞能够被用来抑制在炎性疾病和自身免疫疾病中发生的免疫系统攻击。
Roybal说,“利用synNotch T细胞运送强大的治疗性分子或者直接影响患病位点处的免疫反应将不仅是更加有效的,而且也可能阻止当药物在全身运送时因不加区分地影响身体的每个组织而发生的副作用。治疗性免疫细胞在局部产生分子治疗性药物是一种全新的方法---该方法可能比今天正在使用的全身性药物注射更加有效和更加安全。”
Kole T. Roybal, Jasper Z. Williams, Leonardo Morsut, Levi J. Rupp, Isabel Kolinko, Joseph H. Choe, Whitney J. Walker, Krista A. McNally, Wendell A. Lim.Engineering T Cells with Customized Therapeutic Response Programs Using Synthetic Notch Receptors.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
26
#Cell#
33
#synNotch#
24
继续关注!
65
谢谢分享!
59
#Notch#
31
#OTC#
33
#重磅#
25
謝謝分享,,,
57
學習啦,,
70