PHILIPS每日一例:肝脏原发性鳞状细胞癌一例
2022-09-07 放射沙龙 中华放射学杂志
PSCCL好发于中老年男性,临床症状与体征均无明显特点,亦无特异性肿瘤标志物,其组织起源尚无一致意见。PSCCL罕见,易误诊为肝脓肿,二者的临床症状及体征相似可能与PSCCL合并感染和肿瘤性发热有关。
患者男,49岁。右上腹胀痛2个月,加重伴发热半个月。体检:右上腹有压痛。实验室检查:白细胞计数13.9×109/L (正常参考值4×109-10×109/L),中性细胞数9.1×109/L(正常参考值2.0×109-7.7×109/L);谷氨酰转肽酶72 U/L(正常参考值5~50 U/L);乙肝表面抗体和乙肝核心抗体均阳性,甲胎蛋白和癌胚抗原均无异常。
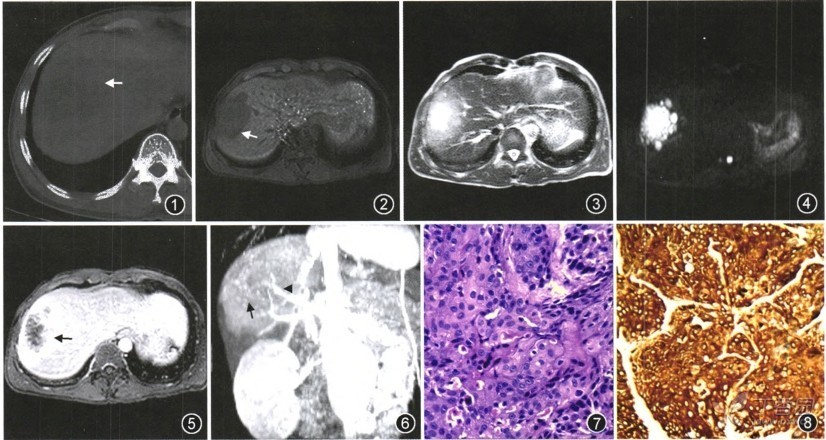
图1 CT平扫示肝脏右叶不规则低密度肿块影,其内见多发结节状更低密度灶,CT值22-48 HU,病灶境界清楚(箭);图2 MR TlWI示肝脏右叶病灶为不均匀中低信号,可见低信号环形带(箭); 图3 MR T2WI示病灶为不均匀中高信号,中间部分信号高于周围; 图4DWI示肿块呈明显高信号的大小不一多房状结构堆积成团;图5延迟增强T1WI示肿块中央轻度强化,周围渐进性强化,其内见不规则线状强化,子灶不均匀强化,邻近肝组织明显强化(箭); 图6 MIP重组像示载瘤动脉增粗扭曲(箭头),瘤内紊乱、管腔粗细不均的新生血管,呈异常扩张扭曲(箭); 图7光学显微镜下见鳞癌细胞及间质纤维组织,间质纤维组织增生,间隔包绕形成大小不一的癌巢(HE×200); 图8免疫组织化学广谱角蛋白在肿瘤细胞内黄染,呈阳性表达(免疫组织化学 ×200)
影像检查:B超:肝脏右叶回声欠均匀,可见6.7 cm×5.5 cm的回声异常,内可见0.5~0.8 cm的较低回声。CT:平扫肝脏右叶一个7.0 cm ×6.5 cm×5.0 cm的不规则低密度肿块影,其内见多发结节状更低密度灶,CT值22~48 HU,病灶境界清楚(图1)。
MRI:肝脏右叶一个7.0 cm×7.0 cm×4.5 cm的不规则病灶,平扫T1WI为不均匀中低信号,可见低信号环形带;T2WI为不均匀中高信号,中央信号高于周围;DWI上肿块呈明显高信号的大小不一多房状结构堆积成团;增强扫描病灶中央轻度强化,周围渐进性强化,内见不规则线状强化,周围子灶不均匀强化,邻近肝组织明显强化。MIP重组示载瘤动脉增粗扭曲,瘤内可见紊乱、管腔粗细不均的新生血管,呈异常扩张扭曲(图2~6)。诊断为肝脏右叶恶性肿瘤。
肝脏穿刺后病理:光学显微镜下见鳞癌细胞及间质纤维组织。免疫组织化学检查示广谱角蛋白(CKp)阳性(+),单克隆抗体P63阳性(++),增殖细胞核抗原Ki-67约20%细胞阳性(+)(图7,8)。病理诊断为肝脏原发性鳞状细胞癌(primary squamous cell carcinoma of liver,PSCCL)。
讨论
PSCCL好发于中老年男性,临床症状与体征均无明显特点,亦无特异性肿瘤标志物,其组织起源尚无一致意见。PSCCL罕见,易误诊为肝脓肿,二者的临床症状及体征相似可能与PSCCL合并感染和肿瘤性发热有关。
PSCCL肿块T1WI为中低信号,可见低信号环形假包膜,T2WI为中高信号;增强扫描病灶在动脉早期无明显强化、分隔不规则强化、周围子灶不均匀强化、邻近肝组织明显强化以及病灶持续性增强表现,这些均可见于肝脓肿。MRI上肿瘤的镶嵌结构及分隔状改变在大体病理上是肿瘤内的分隔和不同的组织成分,在延迟扫描上表现为不规则线状或蜘蛛网状强化。
PSCCL在延迟扫描像仍有强化是由于组织学上富含间质纤维组织的缘故。而肝脓肿的分隔为尚未坏死的肝组织或纤维肉芽肿,强化的时相落后于PSCCL;PSCCL的外周强化可能由于肿瘤侵犯、炎症改变所致,还可能与对比剂积聚在肿瘤的间质间隙及滞留在肿瘤血管有关,而肝脓肿病灶周围肝组织强化是周围的充血水肿带强化,范围与平扫相对应。
MIP重组中PSCCL的载瘤动脉增粗扭曲,瘤内新生血管紊乱、管腔粗细不均,呈异常扩张扭曲。这是肝脏恶性肿瘤的特征性征象,借此可以排除炎症性病变肝脓肿。转移瘤无水肿带、发热、白细胞升高等症状,有原发肿瘤病史可与PSCCL鉴别,但最终确诊需依赖病理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












值得学习
27
#原发性#
29
#细胞癌#
29
#iPS#
43