JBJS:肩关节不稳患者后期继发不稳定型损伤风险显著增高
2013-06-09 JBJS dxy
在年轻运动员和体力劳动者人群中,创伤造成的肩关节不稳发生率较高,长期的肩关节不稳容易出现损伤复发,并继发肩关节骨关节炎,通常需要手术干预以获得肩关节的长期稳定。近年有文献报道,患者自诉的有肩关节损伤病史是肩关节后续损伤的一个危险因素,后期发生肩关节损伤的风险要高于正常人群9倍,但作者并没有将肩关节后续损伤特别限定于肩关节不稳定事件。近日由美国学者完成的美国陆军军官学校对肩关节损伤人群长达4年的随访
在年轻运动员和体力劳动者人群中,创伤造成的肩关节不稳发生率较高,长期的肩关节不稳容易出现损伤复发,并继发肩关节骨关节炎,通常需要手术干预以获得肩关节的长期稳定。近年有文献报道,患者自诉的有肩关节损伤病史是肩关节后续损伤的一个危险因素,后期发生肩关节损伤的风险要高于正常人群9倍,但作者并没有将肩关节后续损伤特别限定于肩关节不稳定事件。近日由美国学者完成的美国陆军军官学校对肩关节损伤人群长达4年的随访研究提示:肩关节不稳患者后期肩关节不稳定损伤概率显著增高,相关结论发表在2013年3月份的JBJS Am杂志上。
研究纳入人群来源于2006年7月26至2010年5月22日在美军陆军军官学校就读的学生,期间共1050例参与研究,约714例受试者完成最终随访,714例受试者中,630例男性(88%),和军队院校的总体人口比例相符合。所有受试者均在USMA中建立医疗档案,并在Keller Amary军队医院进行相关评估。
不稳定事件定义为:通过既往史,体格检查,影像学或手术时确定早期存在前脱位的受试者,在随访过程中出现前脱位;或早期存在后脱位的受试者在随访过程中出现后脱位。所有受试者在出现肩关节损伤时接受一份调查问卷,以明确损伤时间,机制及类型。
最长随访时间四年,主要目标是:随访过程中出现的肩关节不稳定事件,受试者在随访过程中出现以下情况,随访即终止:(1)随访过程中受试者出现肩关节不稳定事件;(2)受试者在毕业前因个人原因离开USMA;(3)随访时间到达最终随访时间点。
研究结果显示:
共714例(1428个肩关节)受试者接受最终随访,8个肩关节因既往有手术病史而除外,共剩余1420例肩关节,其中118例受试者自诉有肩关节不稳定病史。在118例受试者中,28例有脱位,76例有半脱位,14例有半脱位和脱位。在随访过程中共发现46例(39例前脱位,7例后脱位,15例发生在既往自诉有肩关节不稳定病史的受试者中)肩关节急性不稳定事件,其中31例(67.4%)受试者最终接受了手术治疗。肩关节不稳定病史受试者的肩关节不稳定事件累计发生率为12.7%(15/118),而既往无肩关节不稳定病史的受试者发病率为2.4%(31/1302)。
单因素Cox比例风险模型分析显示,既往自诉有肩关节不稳定病史的受试者在后期随访过程中出现肩关节不稳定事件的概率是正常人群的5倍(表1),Kaplan-Meier生存评估分析显示相同结果(图1)。
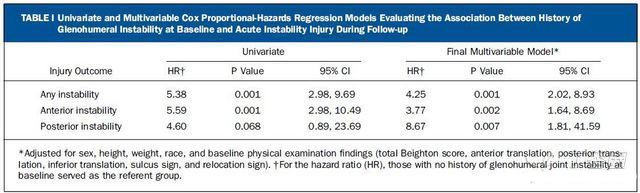
表1:早先肩关节不稳定人群和正常人群随访结果的单因素和多因素Cox 比例风险模型比较
图1:早先不稳定人群和正常人群术后出现肩关节急性不稳定事件Kaplan-Meier生存评估分析。
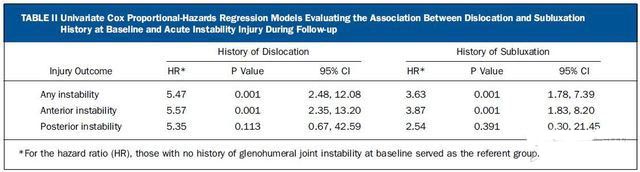
将肩关节前后脱位进行分别统计分析发现,其发生危险性分别是正常人群的5.6倍和4.6倍(图2,3所示);将受试者按脱位和半脱位进行独立危险性统计分析后发现既往存在全脱位的受试者危险性更高(表2)。
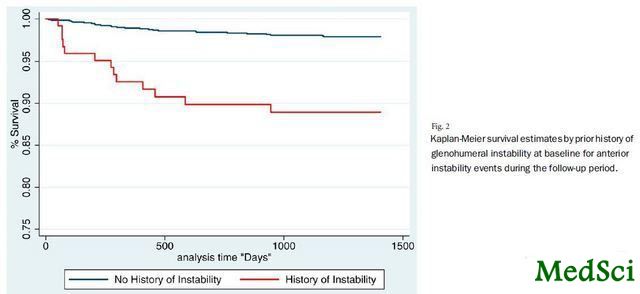
图2:早先前脱位不稳定人群和正常人群术后出现肩关节急性不稳定事件Kaplan-Meier生存评估分析。

图3:早先后脱位不稳定人群和正常人群术后出现肩关节急性不稳定事件Kaplan-Meier生存评估分析。
表2:早先肩关节全脱位和半脱位人群随访结果的单因素和多因素Cox 比例风险模型比较
多因素方差分析得出了相类似的结果。对受试者进行人口学数据和基线水平的调整后发现有肩关节不稳定病史的受试者术后出现肩关节急性不稳定事件的概率是正常人群的4.3倍;对其他相关统计变量进行调整后危险性仍存在持续差异。
作者在研究的最后总结认为:在军事院校这类体力运动强度较大的人群中,既往有肩关节不稳定病史(无论脱位方向和脱位类型)的患者其后出现肩关节急性不稳定事件的概率仍显著高于正常人群。

History of shoulder instability and subsequent injury during four years of follow-up: a survival analysis.
BACKGROUND
Little is known about the risk factors for glenohumeral joint instability. We hypothesized that a prior history of instability would be a significant risk factor for subsequent injury.
METHODS
We conducted a prospective cohort study over a four-year period within a high-risk group of young athletes to address the research hypothesis. Subjects were freshmen entering the U.S. Military Academy in June of 2006. Part of the baseline assessment included documenting a prior history of glenohumeral instability on entry into the study. All subjects were followed for subsequent glenohumeral joint instability events until graduation in May of 2010. The primary outcome of interest in this study was time to glenohumeral instability event during the follow-up period. We examined injury outcomes, looking for any instability, anterior instability, and posterior instability events. Cox proportional-hazards regression models were used to analyze the data.
RESULTS
Among the 714 subjects, eight shoulders were excluded from the analyses due to prior surgical stabilization, leaving 1420 shoulders, of which 126 had a self-reported prior history of instability. There were forty-six (thirty-nine anterior and seven posterior) acute instability events documented in the cohort during the follow-up period. Subjects with a prior history of instability were over five times (p < 0.001) more likely to sustain an acute (anterior or posterior) instability event during the follow-up period. Subjects with a history of instability were also 5.6 times (p < 0.001) more likely to experience a subsequent anterior instability event and 4.6 times (p = 0.068) more likely to experience a posterior instability event during follow-up. Similar results were observed in multivariable models after controlling for the influence of demographic and baseline physical examination findings.
CONCLUSIONS
Despite meeting the rigorous physical induction standards for military service, subjects with a prior history of glenohumeral joint instability were approximately five times more likely to experience a subsequent instability event, regardless of direction, within this high-risk athletic population.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#稳定型#
37
#继发#
38
#肩关节#
39
#损伤#
27
#增高#
29
#增高#
30
#JBJS#
27