Eur Heart J:他汀类药物不耐受的患病率
2022-02-20 MedSci原创 MedSci原创
根据目前对超过400万患者的分析,根据国际定义进行诊断时,SI的患病率很低。这些结果支持这样的概念,即完全SI的患病率可能经常被高估,并强调需要仔细评估与SI相关的潜在症状的患者。
他汀类药物不耐受(SI)是一个重要的公共卫生问题,需要准确估计其患病率。SI仍然是一个重要的临床挑战,它与心血管事件的风险增加有关。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该荟萃分析旨在估计SI的总体患病率、根据不同诊断标准和不同疾病环境的患病率,并确定了可能增加SI风险的可能危险因素/疾病。

研究人员检索了几个数据库,截至2021年5月31日,以确定报告了SI患病率的研究。该研究的主要终点是根据一系列诊断标准[国家脂质协会(NLA)、国际脂质专家小组(ILEP)和欧洲动脉粥样硬化学会(EAS)]和不同疾病环境中的患病率和总体患病率。该研究的次要终点是确定SI的可能危险因素。研究人员应用随机效应模型来估计汇总的SI患病率。

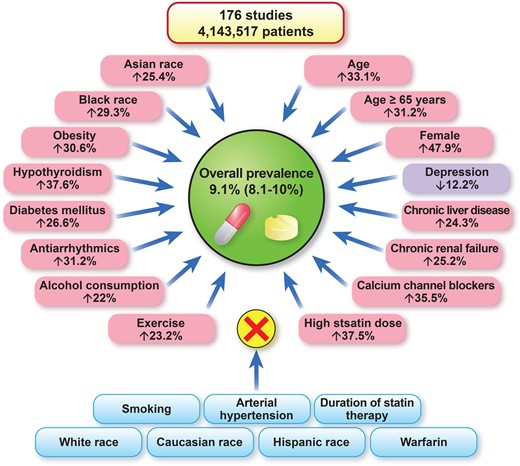
该荟萃分析共有176项研究[112项随机对照试验(RCT);64项队列研究]4143517名患者最终被纳入分析。SI的总体患病率为9.1%(95%置信区间为8.0-10%)。使用NLA、ILEP和EAS标准定义的患病率相似[分别为7.0%(6.0-8.0%)、6.7%(5.0-8.0%)和5.9%(4.0-7.0%)]。与队列研究相比,随机对照试验中SI的患病率显著降低[4.9%(4.0-6.0%) vs. 17%(14-19%)]。在包括一级和二级预防患者的研究中,SI的患病率远高于单独分析一级或二级预防患者时的患病率[18%(14-21%)、8.2%(6.0-10%)、9.1%(6.0-11%)]。他汀类药物的脂溶性不影响SI的患病率[4.0%(2.0-5.0%) vs. 5.0%(4.0-6.0%)]。年龄[比值比(OR)为1.33,P=0.04]、女性(OR为1.47,P=0.007)、亚洲人和黑人(P<0.05)、肥胖(OR为1.30,P=0.02)、糖尿病(在元回归模型中,OR为1.26,P=0.02)、甲状腺功能减退(OR为1.37,P=0.01)、慢性肝功能衰竭和肾功能衰竭(两者的P<0.05)与SI显著相关。抗心律失常药、钙通道阻滞剂、饮酒和增加他汀类药物剂量也与SI风险增加有关。
由此可见,根据目前对超过400万患者的分析,根据国际定义进行诊断时,SI的患病率很低。这些结果支持这样的概念,即完全SI的患病率可能经常被高估,并强调需要仔细评估与SI相关的潜在症状的患者。
原始出处:
Ibadete Bytyç,et al.Prevalence of statin intolerance: a meta-analysis.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac015/6529098
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#不耐受#
34
#他汀类#
66
#他汀类药#
30
学习了
54
#患病率#
52
#ART#
35
#HEART#
36