Br J Cancer:突变型TP53与BCAR1相互作用促进癌细胞的侵袭
2020-11-14 xiaozeng MedSci原创
转录因子TP53作为最重要的肿瘤抑制因子之一,其能够通过调节参与细胞周期停滞、衰老、细胞凋亡、细胞自噬、代谢重编程、肿瘤微环境信号转导以及抑制癌细胞迁移和侵袭的相关靶基因来影响肿瘤的发生发展。
转录因子TP53作为最重要的肿瘤抑制因子之一,其能够通过调节参与细胞周期停滞、衰老、细胞凋亡、细胞自噬、代谢重编程、肿瘤微环境信号转导以及抑制癌细胞迁移和侵袭的相关靶基因来影响肿瘤的发生发展。
TP53信号通路经常由于TP53自身突变或其调节因子(包括CDKN2A,也称为p14ARF和MDM2.8)的改变而失活。大多数TP53突变都是错义突变,可产生稳定且长期存在的蛋白。目前在TP53的DNA结合域内鉴定出许多热点突变,包括R273H。突变型TP53能够与其他蛋白质相互作用并产生有助于癌症转移的功能获得性特性。然而相关的分子机制仍未完全清楚。
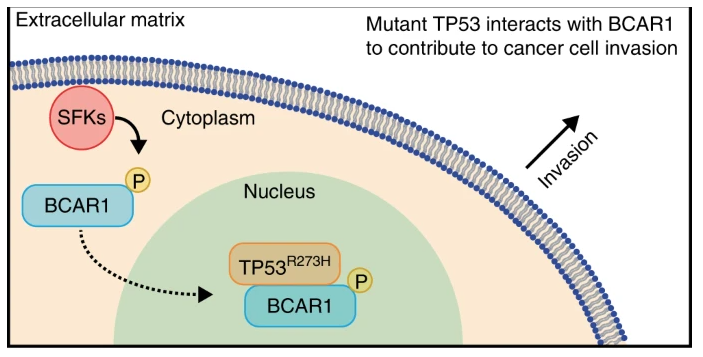
示意图
该研究通过采用免疫沉淀和邻近结扎测定技术,鉴定了BCAR1(乳腺癌抗雌激素抗性1)是TP53R273H突变体的新型结合伴侣。研究人员通过transwell小室实验检查二者结合的相关生物学功能,并在公共数据库中根据TP53状态和BCAR1的表达情况分析患者的临床结局。
TP53R273H与BCAR1相互作用
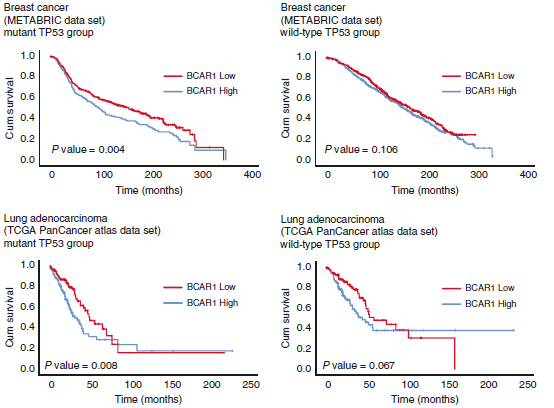
研究人员发现了TP53R273H和BCAR1之间的新型相互作用,BCAR1能够从细胞质转移到细胞核中并以SFKs(SRC家族激酶)依赖性的方式与TP53R273H结合,而后者已知会增强肿瘤细胞的转移。全长的TP53R273H突变体的表达可促进癌细胞的侵袭作用,而BCAR1结合缺陷型的TP53R273HΔ102-207突变体则无此作用。此外,在TP53突变型患者中,BCAR1的高表达水平对应患者较差的预后。
TP53突变型患者中BCAR1高表达对应患者的低总生存率
综上,该研究结果显示,TP53R273H和BCAR1之间的相互作用对于癌细胞的侵袭能力增强起着至关重要的作用。因此,破坏TP53R273H-BCAR1的结合或可成为治疗TP53R273H突变型癌症患者的一种潜在治疗策略。
原始出处:
Guo, A.K., Itahana, Y., Seshachalam, V.P. et al. Mutant TP53 interacts with BCAR1 to contribute to cancer cell invasion. Br J Cancer (04 November 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#相互作用#
37
#突变型#
39
TP53信号通路经常由于TP53自身突变或其调节因子(包括CDKN2A,也称为p14ARF和MDM2.8)的改变而失活。大多数TP53突变都是错义突变,可产生稳定且长期存在的蛋白。
77
#癌细胞#
45
#p53#
48
#TP53#
50
#互作#
31
已读
78