European Radiology:在急诊科就诊的COVID-19患者中,什么水平的D-二聚体可以安全排除肺栓塞?
2022-04-06 shaosai MedSci原创
然而,目前没有指南建议在评估COVID-19患者时常规进行CTPA检查。
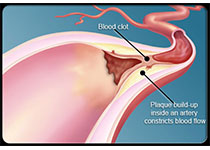
 感染SARS-Cov-2并发展为COVID-19的患者,由于凝血功能的激活亢进,有发生血栓栓塞性并发症的风险。严重的COVID-19病例与炎症和促血栓生物标志物的水平增加有关,如白细胞介素-6和D-二聚体的水平增加。此外,已经证明SARS-COV-2有能力直接感染内皮细胞并诱发血管内皮炎,这也可以促进局部血栓形成。
感染SARS-Cov-2并发展为COVID-19的患者,由于凝血功能的激活亢进,有发生血栓栓塞性并发症的风险。严重的COVID-19病例与炎症和促血栓生物标志物的水平增加有关,如白细胞介素-6和D-二聚体的水平增加。此外,已经证明SARS-COV-2有能力直接感染内皮细胞并诱发血管内皮炎,这也可以促进局部血栓形成。
然而,目前没有指南建议在评估COVID-19患者时常规进行CTPA检查。由于COVID肺炎和PE的症状严重重叠,两者都会造成呼吸困难或饱和度降低,因此评估的复杂性就更大了。
近日,发表在European Radiology杂志的一项研究在急诊科就诊的COVID-19患者中评估了可独立于检测前临床概率而安全排除急性PE的最佳D二聚体水平,为早期诊断PE避免延误疾病治疗提供了数据参考。
本项回顾性研究纳入了2020年3月1日至5月15日期间在AP-HP医院的ED就诊的COVID-19患者,并在就诊后48h内进行了D-二聚体剂量测定及CTPA检查。本研究计算了不同D-二聚体阈值的D-二聚体敏感性、特异性、阳性和阴性预测值,以及假阴性率和失败率,以及可能避免的CTPA数量。
共纳入781名SARS-Cov-2 RT-PCR阳性的患者(平均年龄62.0岁,53.8%为男性),其中60人(7.7%)经CTPA证实为PE。他们的D-二聚体中位数水平明显高于无PE的患者(4,013 vs 1,198 ng-mL-1, p < 0.001)。使用500ng·mL-1,或对大于50岁的患者进行年龄调整后的截断值,其敏感性和净现值都高于90%。在这些阈值下,分别有17.1%和31.5%的CTPA可以被避免。在178名D-二聚体低于年龄调整后的临界值的患者中,有4名患者患有PE,导致可接受的失败率为2.2%。使用更高的D-二聚体临界值可以避免更多的CTPA,但会降低敏感性并增加失败率。

图 D-二聚体诊断性能的ROC曲线分析
总之,本研究支持使用与在普通人群中验证的相同的D-二聚体阈值来安全地排除到ED就诊的COVID-19患者的PE风险。在占COVID-19患者大多数的50岁以上的患者中,应用经年龄调整的阈值可减少三分之一的CTPA检查。
原文出处:
Marie-Pierre Revel,Nathanael Beeker,Raphael Porcher,et al.What level of D-dimers can safely exclude pulmonary embolism in COVID-19 patients presenting to the emergency department?DOI:10.1007/s00330-021-08377-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
32
#二聚体#
36
#急诊科#
46
#COVID-19患者#
49
#D-二聚体#
42