Diabetes Care:阿格列汀可减缓2型糖尿病的颈动脉粥样硬化进展(SPEAD-A)
2015-12-19 Seven L 译 MedSci原创
研究者进行了一项研究,调查二肽基肽酶-4DPP-4)抑制剂阿格列汀在2型糖尿病患者动脉粥样硬化进展中的作用。该多中心前瞻性随机盲法研究纳入了341名2型糖尿病患者,既往没有心血管疾病史,将其随机分为阿格列汀治疗组(n=172)和常规处理对照组(n=169)。以24个月的治疗期间,通过颈动脉超声检查观察到的动脉内膜中层厚度 (IMT)变化为结局指标。研究数据显示,阿格列汀治疗组比对照组降低血糖效果更
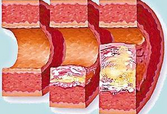
研究者进行了一项研究,调查二肽基肽酶-4(DPP-4)抑制剂--阿格列汀在2型糖尿病患者动脉粥样硬化进展中的作用。
该多中心前瞻性随机、盲法研究纳入了341名2型糖尿病患者,既往没有心血管疾病史,将其随机分为阿格列汀治疗组(n=172)和常规处理对照组(n=169)。以24个月的治疗期间,通过颈动脉超声检查观察到的动脉内膜中层厚度 (IMT)变化为结局指标。
研究数据显示,阿格列汀治疗组比对照组降低血糖效果更优(-0.3 ± 0.7% vs. -0.1 ± 0.8%, P = 0.004),且不会增加低血糖风险。颈动脉最常见IMT区域改变和右侧、左侧颈动脉IMT最大处改变在阿格列汀治疗组比对照组表现优(-0.026 mm [SE 0.009] vs. 0.005 mm [SE 0.009], P = 0.022; -0.045 mm [SE 0.018] vs. 0.011 mm [SE 0.017], P = 0.025, and -0.079 mm [SE 0.018] vs. -0.015 mm [SE 0.018], P = 0.013)。
研究结果表明,对既往无心血管疾病的2型糖尿病患者,使用阿格列汀治疗与常规治疗相比,可减缓该类患者IMT的恶化进展。
原始出处:
Mita T, Katakami N, Yoshii H,et al.Alogliptin, a Dipeptidyl Peptidase-4 Inhibitor, Prevents the Progression of Carotid Atherosclerosis in Patients With Type 2 Diabetes: The Study of Preventive Effects of Alogliptin on Diabetic Atherosclerosis (SPEAD-A).Diabetes Care. 2015 Dec 1. pii: dc150781.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#粥样硬化#
27
#颈动脉#
26
#BET#
25
#Diabetes#
26
谢谢分享。
121
#PE#
31
分享了,
100
不错的文章!
95
哦
118
好东西,值得分享,学习了!
106