Front Oncol:ER+/HER2-且淋巴结阳性的绝经前乳腺癌患者,新辅助化疗(NCT)对比新辅助内分泌治疗(NET)的疗效:III期临床研究NEST
2021-10-05 yd2015 MedSci原创
研究表明,虽然新辅助化疗(NCT)和新辅助内分泌治疗(NET)对患者的预后影响无差异,但是NCT治疗可能避免更多淋巴结切除以及淋巴结阳性更少。
在乳腺癌患者的手术后管理中,淋巴水肿是外科医生最容易遇到和尽量避免的手术并发症。在接受新辅助全身治疗(NST)的患者中,腋部淋巴结的治疗决策变得越来越复杂。而对于ER+/HER2-且淋巴结阳性的乳腺癌患者,新辅助治疗的最佳策略仍需要积极探讨。因此,来自韩国团队开展了NEST (NCT01622361)临床研究,评估ER+/HER2-且淋巴结阳性的绝经前乳腺癌患者,新辅助化疗(NCT)对比新辅助内分泌治疗(NET)的疗效。相关结果发表在Frontiers in Oncology杂志上。
NEST是一项前瞻性、多中心、随机、平行对照III期临床试验,主要评估两组的腋窝淋巴结清除率(ALND),腋窝无复发生存(ARFS)、无病生存期(DFS)和总生存期(OS)。
最终纳入174例患者,其中新辅助化疗(NCT)和新辅助内分泌治疗(NET)均为87例。所以患者均完成24周的新辅助治疗。最终170例患者进行疗效分析。
中位年龄42岁(范围27 54岁)。所有患者均为绝经前患者。65%的患者为临床T2期。94%的患者为G1/2型。少数患者(<5%)为低分化(G3)肿瘤。Ki-67的平均表达在两组之间没有差异(NCT为26.3,NET为26.7,P=0.874)。
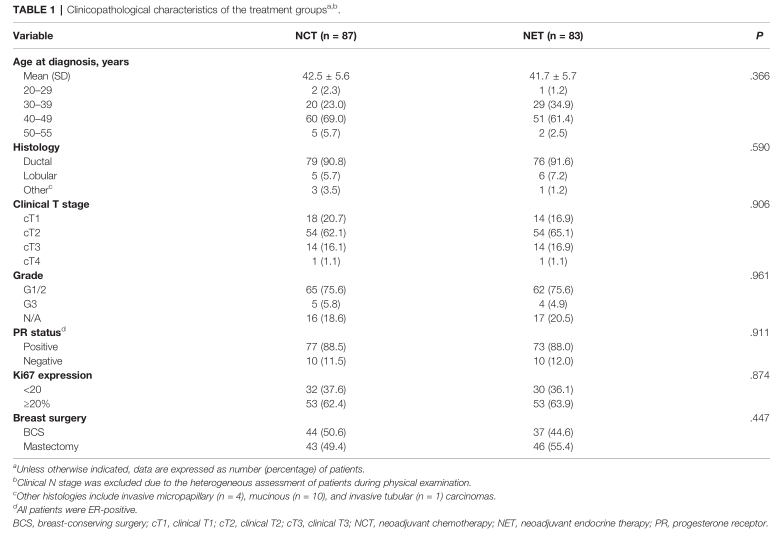
临床特征
49.4%的NCT患者和55.4%的NET患者在治疗完成后进行了乳房切除术,差异无统计学意义(p = 0.447)。NCT组7例(8.0%),NET组1例(1.2%)达到pCR。NCT组有9例(10.3%)患者和NET组有1例(1.2%)患者在乳房中达到pCR。NCT组腋窝淋巴结pCR率明显高于NCT组(13.8% vs. 4.8%,P=0.045)。新辅助治疗后,NCT组的ALND率明显低于NET组(56.3% vs. 71.1%, P=0.046)。此外,与NET组相比,NCT组有更少的LNs被切除(平均,11.74 vs. 14.96, P= 0.003),而且LN阳性率更低(平均,2.92 vs. 4.84, P=0.000)。

疗效评估
在中位随访67.3个月期间,NCT组有19例患者复发转移(局部,n=3;腋窝,n = 3;内乳LN局部复发,n=1;远处转移,n = 12);NET组12例转移(均为远处转移,n=12)。NCT组和NET组的5年ARFS (97.5% vs. 100%,P=0.077)、DFS (77.2% vs. 84.8%, P=0.166)和5年OS (97.5% vs. 94.7%,P=0.304)均没有统计学差异。
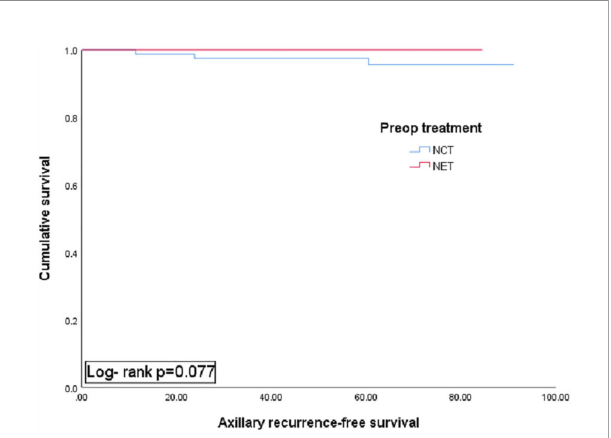
ARFS
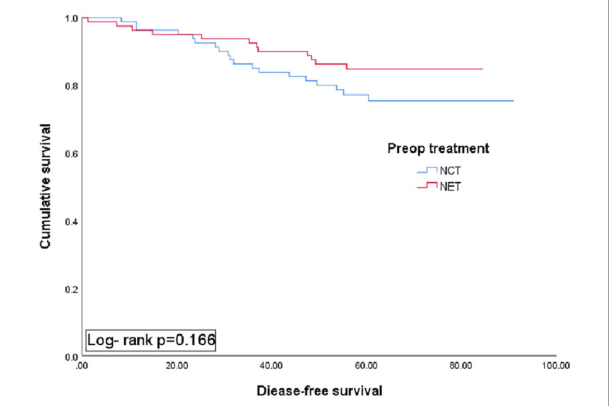
DFS
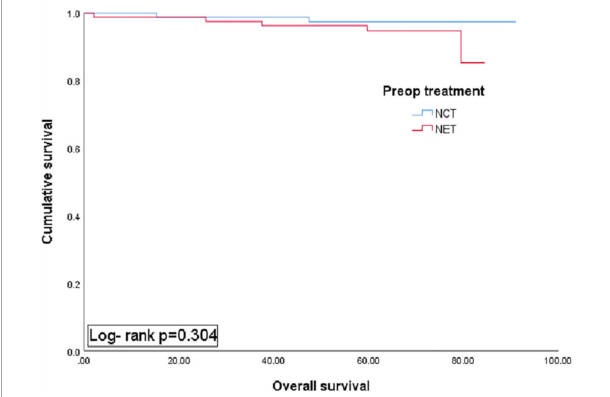
OS
综上,研究表明,虽然新辅助化疗(NCT)和新辅助内分泌治疗(NET)对患者的预后影响无差异,但是NCT治疗可能避免更多淋巴结切除以及淋巴结阳性更少。
原始出处:
Gwark S, Noh WC, Ahn SH, Lee ES, Jung Y, Kim LS, Han W, Nam SJ, Gong G, Kim S-O and Kim HJ (2021) Axillary Lymph Node Dissection Rates and Prognosis From Phase III Neoadjuvant Systemic Trial Comparing Neoadjuvant Chemotherapy With Neoadjuvant Endocrine Therapy in Pre-Menopausal Patients With Estrogen Receptor-Positive and HER2-Negative, Lymph Node-Positive Breast Cancer. Front. Oncol. 11:741120. doi: 10.3389/fonc.2021.741120
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#HER2-#
37
#绝经前#
44
#II期临床研究#
34
#分泌#
29
#新辅助#
31
#III#
32
#NET#
30
#EST#
33
#Oncol#
35
#I期临床#
0