Oncogene:趋化因子受体CCR7促进乳腺癌肿瘤干细胞生长
2015-03-23 佚名 生物谷
近日,来自澳大利亚阿德莱德大学的研究人员在国际期刊oncogene在线发表了他们的最新发现,他们发现趋化因子受体CCR7能够调控乳腺癌中肿瘤干细胞的生长,提示我们CCR7或可成为治疗乳腺癌的一个潜在药物靶点。 趋化因子受体CCR7广泛出现在乳腺癌病理生物学中。虽然最近一些研究表明CCR7高水平表达与晚期肿瘤分级和不良预后具有相关性,但关于其在乳腺癌中的特异性功能及参与的分子机制方面的体内研究仍非常
近日,来自澳大利亚阿德莱德大学的研究人员在国际期刊oncogene在线发表了他们的最新发现,他们发现趋化因子受体CCR7能够调控乳腺癌中肿瘤干细胞的生长,提示我们CCR7或可成为治疗乳腺癌的一个潜在药物靶点。
趋化因子受体CCR7广泛出现在乳腺癌病理生物学中。虽然最近一些研究表明CCR7高水平表达与晚期肿瘤分级和不良预后具有相关性,但关于其在乳腺癌中的特异性功能及参与的分子机制方面的体内研究仍非常有限。
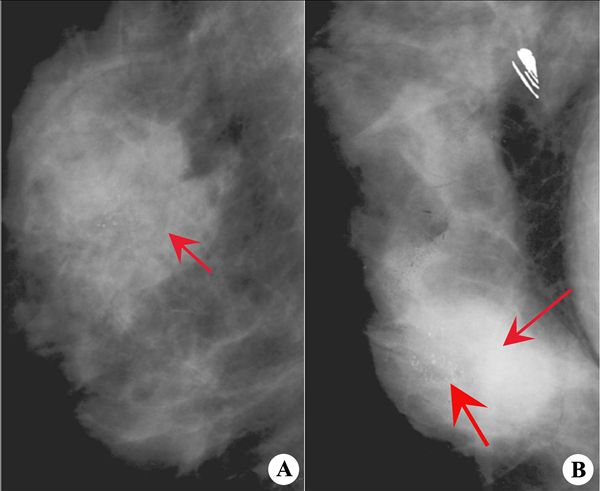
为解决这些问题,研究人员构建了CCR7缺失的乳腺癌小鼠模型,通过观察发现CCR7缺失会导致乳腺癌发生明显迟滞同时伴随肿瘤负荷显著下降。通过对机制研究发现,在人类和小鼠肿瘤细胞中,CCR7能够通过调控具有干性特征的肿瘤细胞发挥功能。体内实验表明通过基因删除或药物阻断的方法抑制CCR7活性能够显著降低小鼠原发性乳腺癌干性细胞的数目,这为CCR7的促肿瘤生长功能提供了一个合理的机制解释。
这些结果揭示了CCR7在乳腺上皮瘤中的癌基因特性,为靶向肿瘤干细胞开发治疗干预手段提供了一个良好的作用靶点。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gene#
39
#趋化因子#
43
#Oncogene#
42
#细胞生长#
42