JACC:经导管主动脉瓣置换后发生脑血管事件的预测因素都有哪些呢?
2016-08-13 MedSci MedSci原创
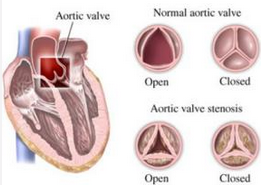
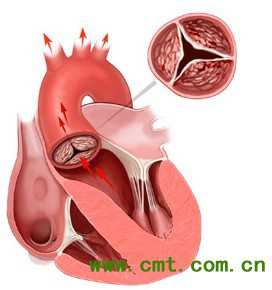
识别处于高危脑血管事件(CVE)风险的经导管主动脉瓣置换(TAVR)患者在具有重要的临床意义。然而,在不同研究中的预测因子都各有不同。本研究的目的是分析TAVR后30天的CVE预测因子。研究人员对报道CVE后TAVR的发病率的研究进行了一项系统性回顾,并且这些研究都提供了感兴趣的预测因子的原始数据。研究人员提取了研究,患者和手术特征的数据,并计算了每个预测因子的粗风险比(RRs)和95%置信区间。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#置换#
29
#JACC#
31
文章很好值得关注
1
#血管事件#
26
#预测因素#
33
#ACC#
29
#主动脉瓣#
27
#主动脉#
27
#经导管#
28
#经导管主动脉瓣置换#
40