Stroke:欧洲烟雾病患者脑部微出血发生率、部位和纵向病程进展与我们有啥不同?
2017-01-07 xing.T MedSci原创
虽然cMBs的发生频率比预期的年龄特异性发病率要高很多,但这还是远远低于以前报道的亚裔烟雾病患者cMBs发生率。这些结果可能反映了确诊的烟雾病患者存在的民族特异性差异。
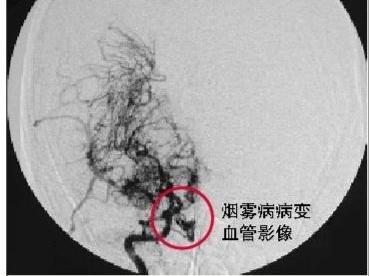
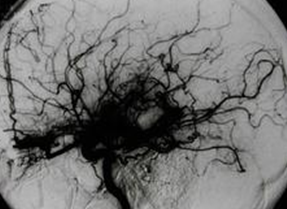
脑部微出血(cMBs)曾在有高出血风险的亚洲烟雾病患者中尤为高发,这大概是烟雾病患者的一个主要特征。近日,卒中领域权威杂志Stroke上发表了一篇研究文章,在此,研究人员回顾性调查了德国一个大型队列中cMBs的发生率、部位和纵向病程进展。
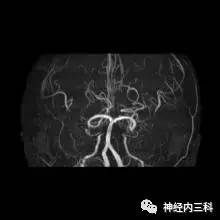
研究人员纳入了从1998年至2015年期间就诊于研究人员所在的医疗科室的所有进行标准的磁共振成像检查的烟雾病患者,包括T2*加权图像。两个独立的研究人员对研究对象的磁共振成像扫描结果进行评估,并根据脑内微出血观测量表来确定cMBs的发生情况。研究者通过图表审查来确定研究对象的人口统计学信息、导致住院的初始症状和相关疾病的情况。
总体而言,101例研究对象共进行了242次T2*加权成像检查,其中烟雾病患者中女性患者占优势(69.3%)。8例患者(7.9%)年龄小于18岁。研究者在13例(12.9%)患者中查出了25处cMBs。1例年龄小于18岁的患者出现cMB;3例颅内出血患者中的2例患者其初始事件表明为cMB(s)。研究人员对101例研究对象中的72例患者进行了1719人次每月的随访,在这个过程中有3例成人查出了3处新发cMBs。大部分(64%)发生cMBs的部位均位于皮质/灰质–白质结合部。
由此可见,虽然cMBs的发生频率比预期的年龄特异性发病率要高很多,但这还是远远低于以前报道的亚裔烟雾病患者cMBs发生率。这些结果可能反映了确诊的烟雾病患者存在的民族特异性差异。
原始出处:
Holger Wenz, et al. Incidence, Locations, and Longitudinal Course of Cerebral Microbleeds in European Moyamoya. Stroke. 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#微出血#
27
#发生率#
39
很好,不错,以后会多学习
70
#欧洲#
39
学习啦,谢谢分享
66
文章很好,拜读受益
69