多篇SCI质疑“β淀粉样蛋白”假说?Nature子刊: 针对可溶性蛋白的新型疫苗,或可逆转老年痴呆!
2021-11-22 网络 网络
阿尔茨海默病的病因向来“迷雾重重”。在诸多假说中,β淀粉样蛋白(Aβ)级联假说最受到认可。然而,基于这一假说的在研疗法纷纷在临床试验中“折戟沉沙”,是否弄反因果,是这种假说的主要争议之一。
阿尔茨海默病(Alzheimer's Disease, AD),俗称“老年痴呆症”,是一类主要发生于老年人且以进行性认知功能障碍和行为损害为特征的中枢神经系统退行性病变。随着人类平均寿命的增长,老年痴呆症的患病率也在不断上升。
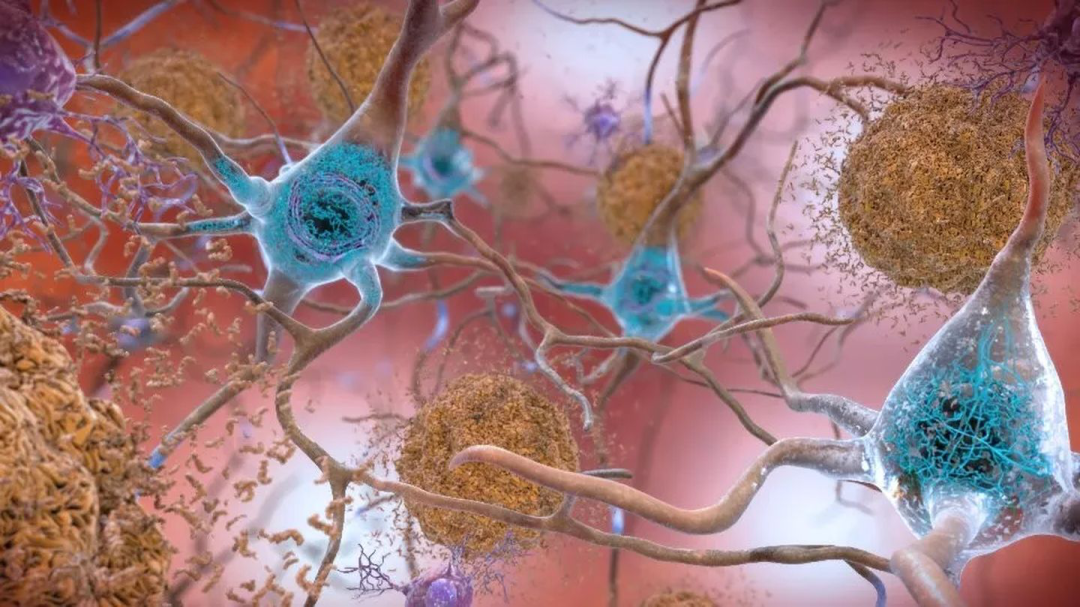
AD的病因向来“迷雾重重”。在诸多假说中,β淀粉样蛋白(Aβ)级联假说最受到认可,脑内淀粉样蛋白斑块的生成也成了AD致病第一大嫌疑人:淀粉样前体蛋白(APP)剪切形成淀粉样蛋白(Aβ),Aβ聚集后形成寡聚体,溶解性变差可沉积成斑块,斑块会导致神经原纤维缠结、神经元丢失等。
然而,基于这一假说的在研疗法纷纷在临床试验中“折戟沉沙”,这让研究人员们不断反思,对“β淀粉样蛋白”的理解是不是错了。是否弄反因果,是这种假说的主要争议之一。
近期,一项发表在Neurology的研究再次引起了对该假说的探讨:“β淀粉样蛋白”可能不是疾病诱因,而是疾病发展的一种结果表现。这项研究的目的就是了解淀粉样变性和神经退行性病变与认知障碍发生的先后顺序。

(图片来源:Neurology)
这项分析从“阿尔茨海默病神经成像计划”中纳入了747名受试者,其中305人认知正常,289人被诊断出轻度认知障碍,153人具有客观定义的细微认知困难(Obj-SCD)——被认为处于认知障碍和痴呆症的非常早期阶段。研究人员对受试者进行了一系列的淀粉样蛋白PET扫描和大脑结构MRI检查。
通过观察四年来的影像检查结果,研究人员发现:相较于认知正常的受试者,出现细微认知困难的人群,大脑中淀粉样蛋白的沉积速度确实更快,但两组的淀粉样蛋白斑块浓度在统计学上并没有差异。细微认知困难人群还出现了大脑内嗅皮层的变薄,这是大脑中与记忆、导航和时间知觉有关的区域。
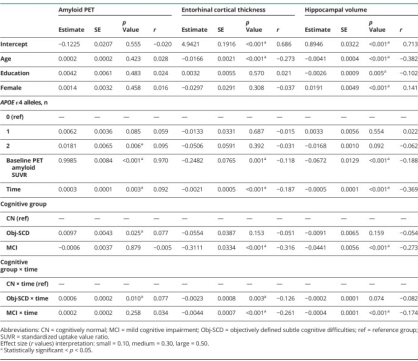
根据认知组状态估计淀粉样蛋白 PET、内嗅皮质厚度和海马体积的变化
(图片来源:Neurology)
因此可以认为,在淀粉样蛋白大量沉积之前,细微认知困难人群的神经退行性病变就已经开始了。
那么,阿尔兹海默病的致病诱因究竟是什么呢?
无独有偶,一项发表在 EClinicalMedicine的研究对该问题进行了全新的诠释——认知障碍可能是由于可溶性淀粉样蛋白β肽的减少而不是淀粉样蛋白斑块的相应积累。
(图片来源:EClinicalMedicine)
研究人员分析了600名参加“阿尔茨海默病神经成像计划”的人脑部扫描和脊髓液,无一例外,这些人都有淀粉样斑块。随后,他们比较了认知正常个体与认知障碍个体的斑块数量和肽水平。令人惊讶的是,无论大脑中斑块的数量如何,具有高水平肽的个体在认知水平上都是正常的。
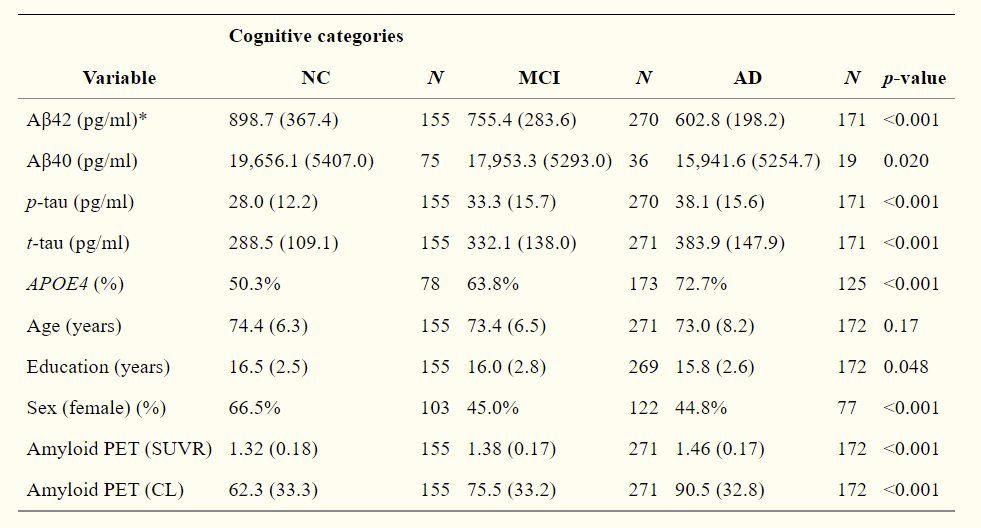
淀粉样蛋白PET阳性个体跨认知类别的脑脊液标志物和基线特征。NC:正常认知;MCI:轻度认知障碍;AD:阿尔茨海默病;Aβ42:42个氨基酸的β淀粉样肽;Aβ40:40个氨基酸的β淀粉样肽
(图片来源:EClinicalMedicine)
除此之外,在 NC中观察到的可溶性Aβ42水平高于 MCI或 AD。较高的可溶性Aβ42水平也与更好的神经心理功能和更大的海马体积有关,后者是大脑中对记忆最重要的区域。
该研究的关键发现是阿尔茨海默病的症状似乎取决于可溶状态蛋白质的消耗,而不是聚集成斑块。该组研究人员也因此认为,阿尔茨海默病计划的未来治疗方法可以着眼于把这些脑可溶蛋白补充到正常水平。
人类对于阿尔兹海默病的疗法一直处于积极探索中。2021年11月15日,来自莱斯特大学、哥廷根大学医学中心和研究慈善机构LifeArc的团队发表在Molecular Psychiatry的研究将治疗的焦点再次锁定在可溶性蛋白。研究人员针对可溶性截短形式的β淀粉样蛋白,开发了一种基于抗体的新治疗方法,以及一种或能预防该疾病的基于蛋白的疫苗。结果显示,不论是治愈方面还是预防方面,新治疗方法和新疫苗都在小鼠模型上减轻了阿尔茨海默病的相关症状。
(图片来源:Molecular Psychiatry)
“在临床试验中,溶解大脑中的淀粉样斑块的潜在治疗方法都没有在减轻阿尔兹海默病的症状方面取得很大成功。有些甚至出现了负面影响。”哥廷根大学医学中心的Thomas Bayer教授解释说,“所以,我们决定采用不同的方法,我们在小鼠体内发现了一种抗体,它可以中和截短形式的可溶性β淀粉样蛋白,但不会与正常形式的蛋白质或斑块结合。”
随后,研究人员改造了这种抗体,使得人类免疫系统不会将其识别为外来物,而是接纳它的存在。当研究到这种名为 TAP01_04 的“人源化”抗体与截短形式的淀粉样蛋白 β 结合的方式和位置时,人们惊讶的发现淀粉样β淀粉样蛋白竟向后折叠起来,形成了一种从未见过的伪β-发夹状结构(pseudo β-hairpin conformation)。
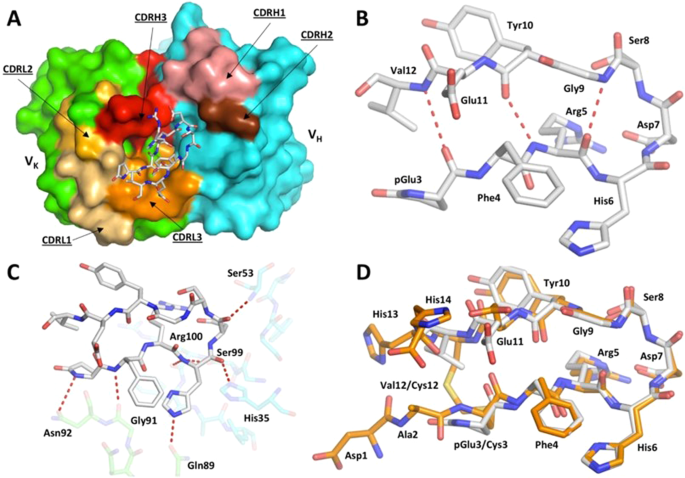
TAP01-Aβ pE3-14复合物的结构
(图片来源:Molecular Psychiatry)
这一独特结构的发现使得研究小组能够设计出该蛋白质区域的一个稳定片段,他们发现该片段也可以形成类似的发夹状结构,并以同样的方式与抗体结合。由此,研究人员设想这种经过改造的β淀粉样蛋白有可能被用作疫苗,以触发接种者的免疫系统产生TAP01_04型抗体。这一想法在小鼠模型上得到了验证。
研究人员随后在两种不同的阿尔茨海默病小鼠模型上测试了“人源化”抗体和改造后的β淀粉样蛋白疫苗(称为TAPAS)。在类似于诊断人类阿尔茨海默病的成像技术的基础上,他们发现抗体和疫苗都有助于恢复神经元功能,增加大脑中的葡萄糖代谢,改善健忘,并且减少β淀粉样蛋白斑块的形成。
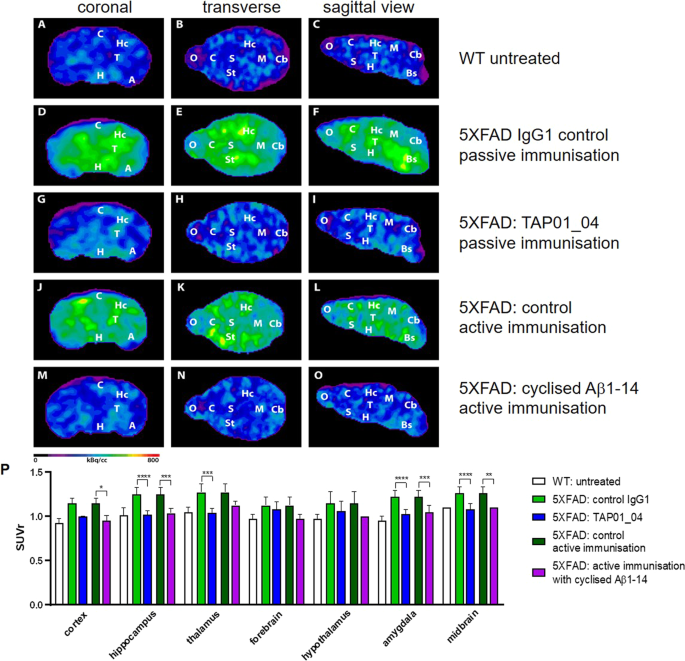
主动和被动免疫减少了5XFAD小鼠的淀粉样蛋白斑块负荷
(图片来源:Molecular Psychiatry)
这项研究的新颖之处在于,人源化抗体TAP01_04和TAPAS疫苗与之前临床试验中测试过的任何阿尔茨海默病抗体或疫苗均有不同,因为它们所针对的是另一种形式的β淀粉样蛋白,这使得它们非常有希望作为治疗性抗体或疫苗。就目前的结果而言,这一成果作为该疾病的潜在治疗方法是非常有希望的。
随着科学的进步,人类对阿尔兹海默病的复杂发病机制愈来愈深入了解,新思想和老观点也在不断的碰撞、摩擦。我们期待,随着对病因和发病过程的不断探讨,能迎来更多对抗阿尔茨海默病的有效手段。
参考资料
[1] Discovery of a novel pseudo β-hairpin structure of N-truncated amyloid-β for use as a vaccine against Alzheimer's disease. Mol Psychiatry. 2021 Nov 15. DOI: 10.1038/s41380-021-01385-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#质疑#
46
#Nat#
38
#淀粉样蛋白#
36
#β淀粉样蛋白#
45
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
41
中位随访时间分别为10.7个月(范围= 0.2
53