BJJ:髋关节后脱位复位后股骨头血供有改变
2013-12-26 佚名 丁香园
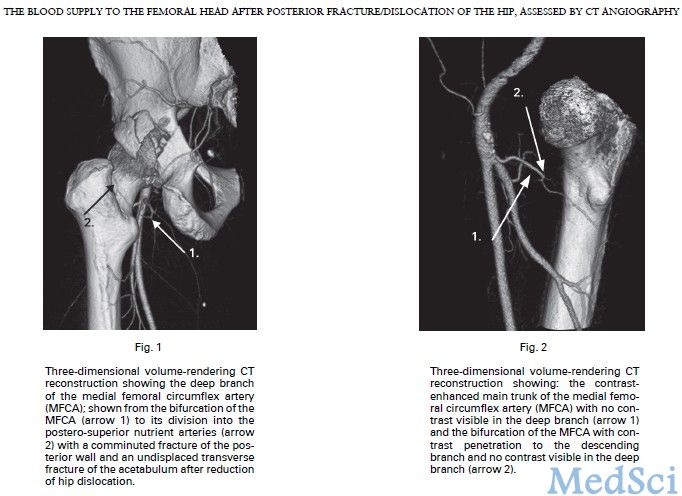
股骨头的血供主要来自旋股内侧动脉(MFCA)及其分支。其中以深支最为重要。股骨头的血供几乎全部来自深支及其终末营养动脉。深支在髋关节后脱位时可受到损伤,根据复位的时间不同,可引发5%-60%的患者发生股骨头坏死。 为了探究髋关节后脱位患者复位后股骨头的血供情况,波兰学者Zlotorowicz等进行了一项研究。 研究人员以35例髋关节后脱位患者的CT-血管造影照片作为研究对象。所有照片均为复位后
股骨头的血供主要来自旋股内侧动脉(MFCA)及其分支。其中以深支最为重要。股骨头的血供几乎全部来自深支及其终末营养动脉。深支在髋关节后脱位时可受到损伤,根据复位的时间不同,可引发5%-60%的患者发生股骨头坏死。【原文下载】
为了探究髋关节后脱位患者复位后股骨头的血供情况,波兰学者Zlotorowicz等进行了一项研究。
研究人员以35例髋关节后脱位患者的CT-血管造影照片作为研究对象。所有照片均为复位后情况。患者的平均年龄为37.1岁(16-64)。在12个月的随访期内,10例患者发生了股骨头缺血性坏死。股骨头坏死患者的髋关节复位时间均在12小时之后(3例患者平均为13小时;7例患者平均为15天)。把之前的正常人股骨头血供研究的55个样本作为对照组,进行卡方检验、Fisher四个表检验以及t检验。
通过分析发现,三组样本(无坏死组、缺血坏死组、对照组)都能找到股骨头三条主要血供:MFCA的深支、起自MFCA的后下侧营养动脉、臀下动脉的梨状肌支。
32例(91%)髋关节后脱位的患者的深支非常明显,而在对照组这一数字为53(96%)(p=0.37)。前者深支的平均直径大于后者的平均直径:1.8 mm(1.1-2.7)vs 1.6 mm(1.1-2.7)(p=0.022)。
后下侧营养动脉一般很细,在对照样本中只有6个(11%)能找到。而在脱位组中有8例找到了该动脉(23%)。在对照组中有27例(49%)找到了臀下动脉的梨状肌支;而在脱位组为9例(26%)。
对股骨头缺血坏死亚组病例的分析发现,8例患者的MFCA深支的平均直径1.8 mm(1.4至2.4);4例患者可找到后下侧营养动脉;1例患者有臀下动脉梨状肌支。
研究人员对以上数据做了进一步分析。由复位后91%的患者可找到深支并且平均直径增大可知:在后脱位复位后,股骨头的血供不仅得到恢复且进一步增加。血流增加的原因可能是缺血后血流重建反应。
三例患者的深支未发现血流:其中两例患者发生了股骨头缺血性坏死(三只主要血管均无血供)。另一例未发生坏死的患者后下侧营养动脉到股骨头的血供增强。
有意思的是,8例股骨头坏死亚组患者的深支血流也得到增加,其可能的原因是坏死骨组织重新获得血供。据此可以猜测,在髋关节脱位时的缺血造成了股骨头的坏死。
臀下动脉梨状肌支的显影的患者相对较少(26% vs 49%)。由此可知,髋关节后脱位和髋关节Kocher–Langenbeck入路都可对其造成损伤。
从该研究可知,CT血管造影是检查髋关节后脱位复位后血供的理想方法,亦有助于预测髋关节后脱位复位后预后即,若三条动脉分支均不显影,则发生股骨头坏死可能性较大。
原文出处:
Zlotorowicz M, Czubak J, Caban A, Kozinski P, Boguslawska-Walecka R.The blood supply to the femoral head after posterior fracture/dislocation of the hip, assessed by CT angiography.Bone Joint J. 2013 Nov;95-B(11):1453-7. doi: 10.1302/0301-620X.95B11.32383.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#后脱位#
38
#骨头#
38
#股骨#
27
#脱位#
24
#股骨头#
30