AACR 2022:奥拉帕利联合环磷酰胺和二甲双胍在子宫内膜癌中表现良好(ENDOLA试验)
2022-04-12 网络 网络
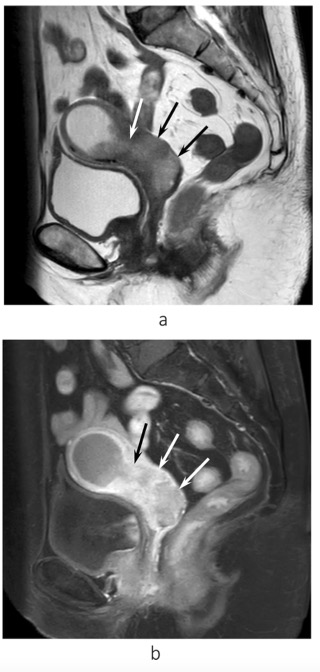
子宫内膜癌主要发生在50至60岁的绝经后妇女,是最常见的妇科癌症之一,在女性癌症的发生率上排名第四,在年龄调整死亡率方面排名第八。根据GLOBOCAN 2012数据库显示,全球子宫体癌的年新发病例为3
子宫内膜癌主要发生在50至60岁的绝经后妇女,是最常见的妇科癌症之一,在女性癌症的发生率上排名第四,在年龄调整死亡率方面排名第八。根据GLOBOCAN 2012数据库显示,全球子宫体癌的年新发病例为319600人,其中发达国家有167900人,发展中国家为151700人。
子宫内膜癌的治疗效果取决于其组织学特征、疾病分级和分期。虽然大多数早期子宫内膜癌可以通过手术治愈(伴或不伴辅助放疗),但是对于晚期或复发的子宫内膜癌来说,其长期的预后却较差,大多数常用的治疗不仅效果不尽如人意,也无法长时间的维持疗效。在以前的前瞻性随机试验中,研究人员已经发现化疗是唯一能够有效提高生存率的辅助治疗措施。因此,不断发展新的化疗方案以改善晚期复发性子宫内膜癌患者的预后就显得相当重要的,目前,单药治疗子宫内膜癌的有效率大约在为4%~27%之间。
2022年AACR年会上,ENDOLA试验(NCT02755844)公布数据表明,奥拉帕利(olaparib)联合环磷酰胺和二甲双胍治疗复发性晚期或转移性子宫内膜癌患者表现出良好的无疾病进展率。
ENDOLA是一项1/2期开放标签、剂量递增试验,在既往接受过多种治疗的复发性晚期子宫内膜癌老年患者中评价奥拉帕尼联合环磷酰胺和二甲双胍节拍治疗。在28天周期内,每6周实施一次剂量限制性毒性(DLT)评估期,最佳剂量确定为与少于20%的患者发生DLT的概率相关的剂量。
在ENDOLA的剂量递增阶段,奥拉帕利在第1周期以150 mg每日两次开始,并递增至300 mg每日两次。使用连续重新评估方法,然后证实推荐的2期试验剂量为300 mg olaparib每日两次、50 mg环磷酰胺节拍治疗每日一次,以及500 mg二甲双胍每日三次。二甲双胍作为抑制P13K通路和减少IGF1循环以及该通路活化而被采用,组成三药联合方案。
在1期研究中,5.9%的患者发生了剂量限制性毒性。具体而言,在150 mg 奥拉帕尼剂量水平下,他们在第1周期发生了3级疲乏。在入组的35例患者中,31例患者可评价-17例患者在1期,14例患者在2期。大多数患者患有子宫内膜样癌(58.1%),而其余患者患有浆液性癌(11%)或癌肉瘤(6.5%)。大多数患者既往未接受过放疗(93.5%)或免疫治疗(93.5%)。此外,一些患者既往接受过内分泌治疗,包括醋酸甲地孕酮(9.6%)、他莫昔芬(6.5%)或芳香化酶抑制剂(12.9%)。
值得注意的是,中位年龄为69岁(46-80岁),超过一半的患者人群既往接受过至少4线治疗(4-5线,25.8%;≥6,29%)。
在试验2期部分对该剂量的评价中,14例可评价患者的10周无进展率为61.5%(95%CI,42.8%-80.2%)。总缓解率(ORR)为20.8%,疾病控制率为66.6%。
除了确定三药联合治疗的推荐2期试验剂量外,研究1期部分的其他主要终点是安全性、剂量限制性毒性和治疗相关不良反应(TRAE)。
在超过10%的可评价患者中观察到TRAE。值得注意的TRAE包括:乏力/疲乏(所有级别,61.3%;3/4级,12.9%)、淋巴细胞减少症(所有级别,38.7%;3/4级,32.3%)、中性粒细胞减少症(所有级别,32.3%;3/4级,16.1%)和血小板减少症(所有级别,29.0%;3/4级,6.5%)。
12例患者(38%)降低剂量,其中9例至少降低2次。2例患者(6%)因毒性中止研究治疗。
在2期部分,研究者评价了10周时的无进展率。原假设是 20% 的 P0,备择假设为P1至少为50%。在第一阶段,10例患者中,至少需要3例成功继续进入第二阶段。在第二阶段,17例患者中至少需要6例试验成功才能被视为阳性。每隔一个周期进行一次影像学评估。
值得注意的2期部分的次要终点为无进展生存期(PFS)。中位PFS为5.1个月(95%CI:3.7-8.1);具体而言,子宫内膜样癌患者的中位PFS为7.5个月(95%CI:5.1-8.9),浆液性癌患者的中位PFS为4.3个月(95%CI:2.7-5.8)。
研究者进一步将PFS数据与KEYNOTE-755试验(NCT03517499)的数据进行了比较,其中既往接受过至少1种铂类药物化疗方案的晚期子宫内膜癌患者接受了20 mg乐伐替尼(Lenvima)每日一次口服给药加200 mg帕博利珠单抗(Keytruda)每3周一次静脉给药(n=411),或医生选择的化疗(n=416)。在这项3期试验中,接受联合治疗的患者的中位PFS为7.2个月(95%CI,5.7-7.6),单独化疗为3.8个月(95%CI,3.6-4.2)(HR,0.60;95%CI,0.50-0.72;P<0.001)。ORR为31.9%(95%CI,27.4%-36.6%)vs 14.7%(95%CI,11.4%-18.4%)。具体而言,对于子宫内膜样癌患者,中位数为7.6个月,浆液性癌患者为5.7个月。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内膜#
41
#环磷酰胺#
64
#ACR#
63
#AACR#
47
感谢分享
63
完美
58