PHILIPS每日一例:胸膜上皮样血管内皮瘤1例
2022-09-05 放射沙龙 中华胸心血管外科杂志
上皮样血管内皮瘤是一种少见的起源于血管内皮细胞的恶性肿瘤,WHO(2002年)新分类列入软组织肿瘤中的恶性脉管肿瘤。
患者女,51岁。无明显诱因左胸部针刺样疼痛1年,间歇性发作。CT检查结果见图1~3,左侧胸廓缩小,纵隔左移;左侧胸膜弥漫性不均匀增厚,增强后轻度强化,内见液性包裹;左肺见斑条状密度增高影,与左侧胸膜相连,边界欠清。
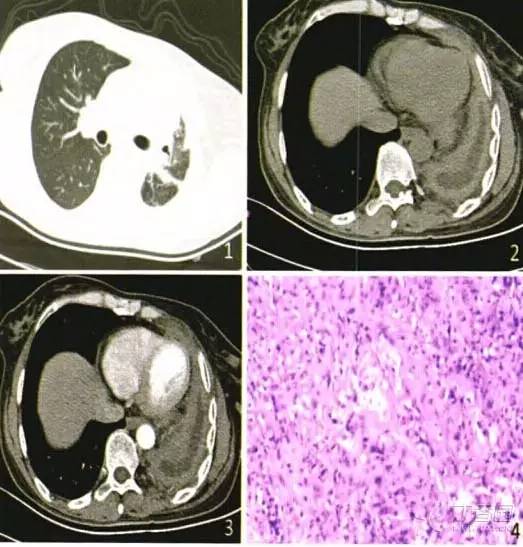
图1肺窗示左侧胸廓明显缩小,左肺可见斑条状高密度影,边界尚清;图2纵隔窗示左侧胸膜弥漫性不均匀增厚,内见弧形包裹性积液;图3增强扫描增厚的胸膜轻度较均匀强化,其内液性低密度区未见明显强化;图4左侧胸膜活检病理示左胸膜上皮样血管内皮瘤
2013年2月行全麻下脓肿清除+胸膜活检术。术中见左侧胸膜广泛增厚,质地坚韧,内见包裹性囊腔,引流淡黄色液体约300 ml;脏层纤维板与肺实质分界不清,与纵隔及心包紧密粘连,无法剥离,行胸膜活检术。病理结果示左胸膜上皮样血管内皮瘤(图4)。免疫酶标记:钙结合蛋白(-),间皮细胞(-),细胞角蛋白7(-),细胞角蛋白20(-),甲状腺转录因子-1(-),雌激素受体(-),孕激素受体(-),癌胚抗原(-),角蛋白抗原决定簇CAM 5.2灶(+),波形蛋白(+),跨膜糖蛋白CD34(+),血小板内皮细胞黏附分子CD31(-),细胞增殖相关抗原Ki67(+)5%。
患者术后出院。电话随访,左侧胸痛症状加重,伴胸闷气急,时有咳嗽咯痰,左侧胸廓变形、塌陷加重。
讨论
上皮样血管内皮瘤是一种少见的起源于血管内皮细胞的恶性肿瘤,WHO(2002年)新分类列入软组织肿瘤中的恶性脉管肿瘤。以原始血管形成为特征性病变,多见于骨、肝、软组织及肺等处。原发于胸膜的上皮样血管内皮瘤极为少见,常见于老年男性,临床症状常表现为胸痛、胸闷及咳嗽。
上皮样血管内皮瘤组织形态结构多变,极易误诊,典型表现为患侧胸膜病变广泛,呈弥漫性均匀增厚或结节样不均匀增厚,多伴有胸腔积液,常构成胸腔瘤性韧而坚实的纤维板状实性肿块,胸膜肥厚,纤维板性粘连,胸腔消失。肿瘤破坏壁层、脏层胸膜,累及肺形成结节。本例左肺内见斑条状密度增高影,不除外左肺受累。另外,患侧胸廓缩小也是常见征象阻。胸膜上皮样血管内皮瘤应与结核性胸膜炎、弥漫型恶性胸膜间皮瘤和胸膜转移性肿瘤鉴别。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#胸膜#
48
#iPS#
47
#上皮样#
49