CSBB:新型纳米颗粒或有效治疗机体炎性肠病
2016-04-18 生物谷 生物谷
最近,刊登于国际杂志Colloids and Surfaces B:Biointerfaces上的一项研究论文中,来自乔治亚州立大学和中国西南大学的研究人员通过联合研究开发了一种新型纳米颗粒可以有效阻断在炎性过程中扮演关键角色的细胞表面分子,这种新型纳米颗粒或可作为炎性肠病(IBD)的一种安全性疗法。 这种纳米颗粒可以减少CD98的表达,CD98分子是一种促进炎症发生的糖蛋白,研究者Didier
最近,刊登于国际杂志Colloids and Surfaces B:Biointerfaces上的一项研究论文中,来自乔治亚州立大学和中国西南大学的研究人员通过联合研究开发了一种新型纳米颗粒可以有效阻断在炎性过程中扮演关键角色的细胞表面分子,这种新型纳米颗粒或可作为炎性肠病(IBD)的一种安全性疗法。
这种纳米颗粒可以减少CD98的表达,CD98分子是一种促进炎症发生的糖蛋白,研究者Didier Merlin教授说道,我们的研究结果表明,纳米颗粒或可潜在作为一种有效的治疗炎症的疗法,我们之所以靶向作用CD98分子是因为此前研究中我们发现CD98分子在参与IBD的活性免疫细胞中处于高度表达的状态。
在美国有230万人受IBD疾病的困扰,IBD包括溃疡性结肠炎和克罗恩病,症状主要表现为慢性或复发性的机体免疫系统异常反应以及胃肠道的炎症等;IBD随着时间变化症状会不断加剧,而且会引发急性的胃肠道症状,比如持续性腹泻、抽筋腹痛、直肠出血等,当药物不能够对这些症状进行控制时就需要进行手术了,同时患者患结肠癌的风险还会增加。
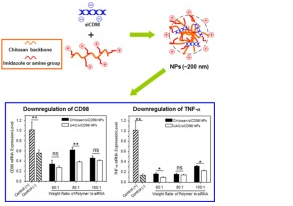
研究者指出,开发纳米治疗策略或可替代当前很多药物来有效抑制IBD的发生和恶化;本文研究中研究者通过结合CD98 siRNA开发出了这种纳米颗粒,siRNA可以通过利用尿刊酸修饰的壳聚糖(UAC)来抑制巨噬细胞中CD98基因的表达,壳聚糖是一种来自贝壳外壳中的多糖物质,当引入巨噬细胞后,纳米颗粒就会对免疫细胞产生一种抗炎症效应。
最后研究者发现,这种纳米颗粒存在一定合适的尺寸,而且不会对巨噬细胞和结肠上皮细胞产生明显的毒性效应,细胞研究结果显示,携带重量比60:1(UAC:siCD98)的纳米颗粒具有最佳的抗炎性效力。
原始出处:
Bo Xiaoa, Panpan Maa, Emilie Viennoisb, c, Didier Merlinb, c,et al,Urocanic acid-modified chitosan nanoparticles can confer anti-inflammatory effect by delivering CD98 siRNA to macrophages,CSBB,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#纳米颗粒#
0
#有效治疗#
27
文章高大上
144
学习了…
98