病例讨论:转移性右下腹痛、右上腹包块、间断发热
2010-09-12 MedSci原创 MedSci原创
来源:中国医学论坛报 北京大学人民医院 北京大学肝病研究所 郭芳 王豪 饶慧瑛 魏来 病历摘要 患者男性,19岁,“转移性右下腹痛1.5个月,右上腹包块伴间断发热1月”入院。1.5个月前,患者因进食生冷食物后出现恶心、呕吐,剑突下疼痛,之后出现右下腹痛,于当地医院诊断为“急性阑尾炎”,抗感染治疗4天后症状完全缓解。1个月前无明显诱因出现右上腹包块,大小约4.0 cm×5.0 cm,
来源:中国医学论坛报
北京大学人民医院 北京大学肝病研究所 郭芳 王豪 饶慧瑛 魏来
病历摘要
患者男性,19岁,“转移性右下腹痛1.5个月,右上腹包块伴间断发热1月”入院。1.5个月前,患者因进食生冷食物后出现恶心、呕吐,剑突下疼痛,之后出现右下腹痛,于当地医院诊断为“急性阑尾炎”,抗感染治疗4天后症状完全缓解。1个月前无明显诱因出现右上腹包块,大小约4.0 cm×5.0 cm,平静时无疼痛,体位改变时疼痛,同时出现发热,体温多于夜晚升高,最高约38 ℃,伴乏力、盗汗,晨起体温可恢复正常,发热持续1周,之后未再测体温。腹部包块无进行性增大。1周前,患者于我院就诊,查血常规,白细胞为 17.28×109/L,中性粒细胞为 78.7%。红细胞沉降系数为55 mm/h。腹部超声检查显示,肝混合回声包块,其内多发强回声,胆囊壁增厚性改变,胰腺尾部形态饱满,脾稍厚。为进一步诊治,以肝内占位性病变、性质待查收入院。
患者有间断剑突下疼痛伴呕吐病史4年多,间隔数月发作1次,多在进食生冷食物后出现,症状持续1周,口服消食片等可缓解,未规律诊治。否认高血压、冠心病及糖尿病史。否认药物、食物过敏史。否认外伤史、手术史及输血史。否认肝炎、结核病史及密切接触史。预防接种史不详。患者出生并长期居住于内蒙古,无疫区停留史及疫水接触史。无射线、化学毒物及粉尘接触史,不嗜烟酒。未婚,否认家族性遗传病病史及其他相关疾病史。
检查结果
查体 体温37.5 ℃,心率86 次/分,呼吸16 次/分,血压120/70 mmHg,发育正常,自动体位,步入病房。神志清楚,全身皮肤、黏膜无黄染,无出血点及皮疹,未见肝掌、蜘蛛痣。全身浅表淋巴结无肿大及压痛。球结膜无苍白、巩膜无黄染。口唇无苍白、发绀,颈无抵抗,颈静脉无怒张,甲状腺无肿大,气管居中,胸廓无畸形,双侧呼吸运动对称。双肺呼吸音清,未闻及干湿音。心前区无隆起,心率86次/分,律齐,各瓣膜听诊区未闻及病理性杂音及心包摩擦音。
右上腹靠近中线部位可见1个4.0 cm×5.0 cm的膨出,无搏动。右侧腹肌紧张,有压痛、无反跳痛,莫非征阴性,麦氏点无压痛。肝、脾脏肋下未触及。全腹叩诊呈鼓音,肝上界位于右锁骨中线第V肋间叩浊,脾区无叩击痛,移动性浊音阴性。双肾区无叩痛。肠鸣音为4 次/分,腹部无血管杂音。脊柱四肢无异常,神经反射正常。
实验室检查
外周血白细胞为16.701×109/L,中性粒细胞为77.63 %,淋巴细胞为14.52 %,嗜酸性粒细胞为0.70 %,单核细胞为7.10 %,嗜碱性粒细胞0.10 %,血红蛋白为130 g/L,血小板为231×109/L。丙氨酸氨基转移酶(ALT)为107 U/L,天冬氨酸氨基转移酶(AST)为64 U/L,碱性磷酸酶(ALP)为120 U/L,转肽酶为95 U/L,总胆红素为9.4 μmol/L,总蛋白为69.9 g/L,白蛋白为36.6 g/L,总胆固醇为2.69 mmol/L,甘油三酯为0.58 mmol/L,血糖5.71 mmol/L。凝血酶原时间为13.20 s,凝血酶原活动度为71.0 %。红细胞沉降率为61 mm/h。血钾为4.55 mmol/L,血钠为134.5 mmol/L,血氯为95.6 mmol/L,二氧化碳结合力为23.5 mmol/L。类风湿因子为20.0 IU/ml,抗链O 为300 IU/ml,免疫球蛋白IgA为 2.51 g/L,IgG 为14.8 g/L,IgM为 1.17 g/L,补体C3为 1.73 g/L,补体C4为 0.276 g/L。甲胎蛋白为1.88 ng/ml,C反应蛋白为110 mg/L。抗HIV及抗HCV均阴性,HBsAg阴性,HBsAb为363.17,梅毒抗体阴性。
影像学检查
CT检查显示,肝方叶下部局部彭隆,形成范围约5.5 cm×4.6 cm的软组织影,内部密度不均,有分隔,可见少许气体,低密度区CT值约31 Hu,前缘与右侧腹直肌分界不清,增强扫描,病灶边界变清晰,分隔明显强化,强化程度与周围正常肝脏强化程度相近,内部低密度区不强化。
余肝脏大小形态正常,肝内胆管无扩张。胆总管上端稍粗,直径约9 mm,逐渐变细,壁均匀。
腹腔内未见积液,腹主动脉旁可见数个类圆形相对低密度影。
胆囊、胰腺、脾脏及肾脏CT检查无异常。
CT印象:① 肝方叶部位占位,考虑脓肿形成,侵犯右侧腹直肌;② 腹主动脉旁淋巴结肿大(图1、2)。
超声检查显示,肝脏形态正常,肝右叶最大斜径14.1 cm,左肝剑下径7.0 cm,包膜光滑,边缘锐,实质回声均匀,肝内血管走行清晰,左肝内可见1个5.0 cm×4.0 cm混合包块,其前缘向被膜外膨出,肝内胆管无扩张。门静脉主干内径为1.0 cm。
胆囊为8.1 cm×2.2 cm,壁毛糙,壁厚0.7 cm,腔内可见多个漂浮光点,胆总管为0.5 cm。脾脏为9.5 cm×3.3 cm,肋下为0(侧位),脾内回声均匀(图3)。

图1 腹部CT平扫影像

图2 腹部CT增强扫描影像
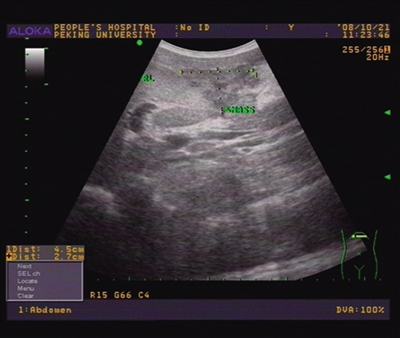
图3 穿刺抽脓前的腹部超声结果
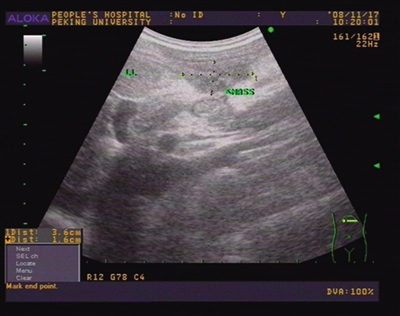
图4 穿刺抽脓后的腹部超声结果
入院诊断:肝内占位性病变性质待查 占位性病变性质?肝脏占位性病变主要有肝脏肿瘤、肝包虫病和肝脓肿(细菌性和阿米巴肝脓肿)。 肝脏肿瘤?肝包虫病?
该例患者否认既往慢性肝病病史。发现肝区包块,伴有乏力、发热、盗汗,存在肝脏肿瘤如原发性肝癌、肝淋巴瘤及肝转移癌可能。患者虽来自肝包虫的高流行地区,出现右上腹包块伴发热,但腹部包块硬,无囊性感,故不支持肝包虫病诊断。
细菌性肝脓肿?
细菌性肝脓肿是指化脓性细菌引起的感染。肝脏接受门静脉和肝动脉双重供血,并通过胆道与肠道相通,因而感染的发生危险高。但是,肝脏的供血丰富,并有具有强大吞噬功能的单核-吞噬细胞系统,因此,细菌性肝脓肿临床上并不经常发生。
细菌性肝脓肿常见致病菌有大肠杆菌、链球菌、葡萄球菌及厌氧菌。该病如未能得到及时有效治疗,可发生脓肿破入胸腔或腹腔,形成脓胸、腹膜炎、膈下脓肿、脓毒症等严重并发症。细菌性肝脓肿的诊断依据如下。
1. 症状与体征
患者起病较急,早期常见寒战、高热,体温38℃~40℃,呈弛张热,反复发作。肝区疼痛,乏力、纳差、恶心、呕吐、腹胀,可有黄疽。
查体可见右季肋区饱满,肝区压痛和肝肿大最常见。肝区叩击痛,右上腹腹肌紧张,肋间隙可因皮肤肿胀而视诊界限不清。
2. 辅助检查手段
血常规:白细胞增多,可达20~30×109/L,中性粒细胞增多,并有核左移或有毒性颗粒。危重患者白细胞可不升高。
超声检查:可见肝内液性暗区,并显示脓腔大小、部位及距体表的距离。超声还可引导穿刺确诊。
X线检查:肝脏阴影增大,右膈升高、活动受限,或有右肺不张、胸腔积液。立位片可见脓腔内气液面。
治疗
CT检查:CT检查有助于确定脓肿的大小及形态。CT主要表现为肝内出现低密度区,CT值略高于肝囊肿,边界多数不太清晰,有时低密度区内可出现块状影。注射造影剂后,其外围增强明显,边界更加清楚。增强扫描的典型表现是脓肿壁的环状增强(靶征),出现“靶”征强力提示脓肿已形成。
磁共振成像(MRI)检查:脓肿形成后,在MRI检查的T1权重像上为低强度信号区;在T2权重像上,脓肿和水肿的组织信号强度增高明显,在其间可存在稍低信号强度的环状脓肿壁。
试验性肝穿刺超声检查:该检查手段有助于确定脓肿的大小、部位以及距局部皮肤的最近距离,选择最佳穿刺点。抽到脓液后,应立即送细菌培养(应包括厌氧菌培养),并进行药物敏感试验。
本例患者的诊断:综合本例的患者主要临床表现、体征、实验室及影像学指标,患者主要有以下特点。
● 患者有 “急性阑尾炎”病史,因此有病原菌侵入肝脏的可能途径。
● 患者出现发热症状
● 体征表现为右上腹靠近中线部位可见一个4.0 cm×5.0 cm大小膨出、无搏动,右侧腹肌紧张,有压痛。
● 实验室检查同样符合感染征象,外周血白细胞为16.701×109/L,中性粒细胞为77.63%,淋巴细胞为 14.52%。
● 影像学检查提示肝脏方叶脓肿形成。
根据上述临床特征,确定该患者的诊断为细菌性肝脓肿。细菌性肝脓肿治疗手段包括非手术治疗和手术治疗。
细菌性肝脓肿 非手术治疗
1. 全身支持疗法
细菌性肝脓肿往往因为病程长,高热消耗等因素,多数患者可出现严重的营养不良、贫血、低蛋白血症、水电解质失衡等。应及时予以补充足够的热量、纠正电解质失衡。
2. 抗生素治疗 应使用较大剂量的抗生素,并根据细菌培养结果和药敏试验结果来选择抗生素。
3. 经皮肝脓肿穿刺引流术 该治疗既可作为诊断手段,又可作为一种治疗方法。
经皮肝穿刺引流术可以确定脓肿的性质,鉴定是否为细菌性或阿米巴性肝脓肿。超声或CT定位引导均可,但B超引导最好,对患者没有损伤。使用超声穿刺专用探头可全程监视穿刺过程,定位准确,还可以随时调整穿刺位置,提高穿刺成功率。尤其是对于多腔脓肿,超声全程引导穿刺可准确进入脓腔,分别抽吸,具有无可比拟的优点。
脓肿穿刺时,尽量抽尽脓液后,可用生理盐水反复冲洗脓腔,然后注入敏感的抗生素,可以取得良好疗效。待治疗到冲洗出液体变清澈,超声检查脓腔变小,基本无液性暗区,即可拔管。对脓腔较大者,可沿穿刺针方向置入导管,持续引流加上间断冲洗。必要时扩张窦道,放入较粗的导管保证引流通畅。该治疗手段简单、安全,可重复操作,成功率可达80%,目前已得到广泛应用。
细菌性肝脓肿 手术治疗
1. 脓肿切开引流术 对于肝左叶脓肿,肝右前叶下方脓肿,胆源性肝脓肿,伴腹肌紧张和腹膜刺激症状明显,拟诊为脓肿破入腹腔者,应积极进行脓肿切开引流术。
2. 肝叶切除术 用于病期长的慢性厚壁肝脓肿、肝脓肿切开引流后残留死腔或窦道长期不愈、肝内胆管结石合并左外叶多发性肝脓肿而该叶肝组织破坏严重,失去正常生理功能者。
患者治疗经过 患者入院后仍有发热,体温最高达39℃。血清白蛋白数值在正常值低限,伴肝脏生物化学指标异常。治疗方案包括以下几项。
● 加强营养,改善一般状况。
● 应用头孢哌酮舒巴坦钠 (2 g bid),联合甲硝唑(0.915 g bid)抗菌治疗。
● 甘草酸二胺静脉输注(100 mg/d)保肝治疗。
● 给予超声引导下穿刺抽脓,顺利抽出脓液,呈黄绿色,黏稠,共抽取脓液共40 ml,抽取后无回声区1.3 cm×1.0 cm。
脓液培养为甲型溶血性链球菌。药敏结果显示头孢唑啉、头孢哌酮、头孢西丁、左氧氟沙星、复方新诺明及万古霉素均敏感,红霉素耐药。1周后再次进行超声引导下穿刺抽脓,抽取脓液共20 ml,生理盐水反复冲洗脓腔。 第一次穿刺抽脓后患者体温恢复正常(入院第5天),仍诉体位改变后右上腹疼痛,无恶心呕吐,食欲,睡眠好。右上腹包块轻压痛,无肝区叩痛。 第二次穿刺抽脓后体位改变右上腹疼痛不明显,右上腹可及3×3.0cm包块,包块处无明显压痛,无肝区叩痛。复查的结果显示,白细胞为 7.580×109/L,中性粒细胞为57.20%。ALT为 48 U/L,AST为21 U/L,总蛋白为73.5 g/L,白蛋白为44.8 g/L,胆固醇为4.40 mmol/L,甘油三酯为1.10 mmol/L。超声检查提示肝内有3.6 cm×1.6 cm实性低回声,无液化征象(D7版图4)。
患者出院。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#包块#
45
#病例讨论#
61
#间断#
39
#腹痛#
50
#转移性#
57