Sci Transl Med:颠覆常识!化疗反而增加了乳腺癌转移风险
2017-07-12 佚名 学术经纬
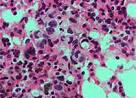
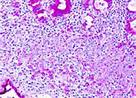
在人类与癌症抗击的历程中,化疗是被我们使用了很久的一种武器。通过化学药物来抑制细胞分裂,患者的病情往往能得到立竿见影的控制。因此,在乳腺癌的治疗中,医生们往往会先对患者进行化疗,抑制患者肿瘤的生长,然后再进行手术,切除病灶。在所有人看来,这是最保险的治疗手段。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Transl#
29
#转移风险#
35
#TRA#
34
#癌转移#
33
#Med#
28
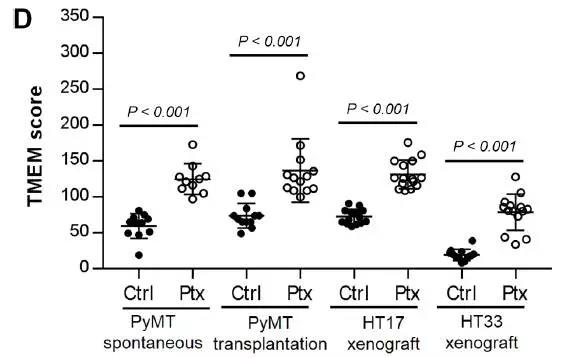
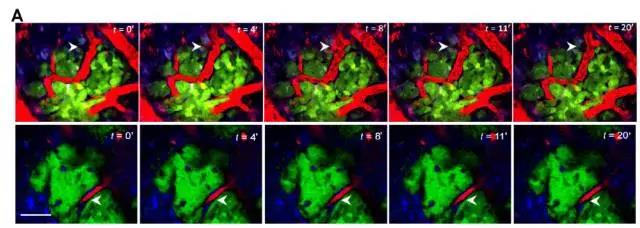
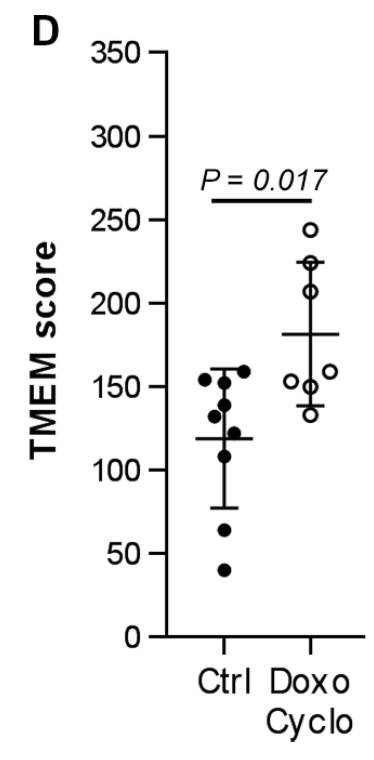
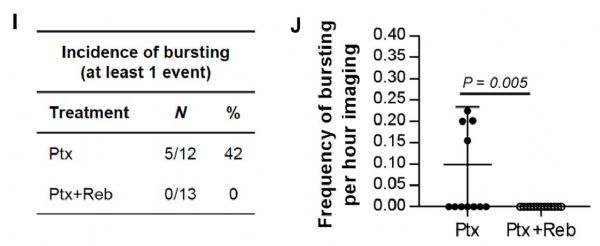
新辅助化疗增加乳腺癌的转移,
71
学习了,谢谢分享
68