JACC:颈动脉支架术后脑缺血损伤加大未来脑血管风险
2015-02-23 张旭栋 MedSci原创
颈内动脉粥样硬化后狭窄,进行颈动脉支架术(CAS)或颈动脉内膜切除术血运重建(CEA)后,MRI显示存在围手术期缺血性损伤。国际颈动脉支架研究(ICSS)对有症状的颈动脉狭窄患者进行CAS与CEA之间的比较。ICSS-MRI组,50%患者行CAS,17%患者行CEA,术后一天弥散加权成像显示存在围手术期缺血性损伤(调整后优势比5.21;95%可信区间:2.78-9.79:P<0.0001)。
颈内动脉粥样硬化后狭窄,进行颈动脉支架术(CAS)或颈动脉内膜切除术血运重建(CEA)后,MRI显示存在围手术期缺血性损伤。国际颈动脉支架研究(ICSS)对有症状的颈动脉狭窄患者进行CAS与CEA之间的比较。ICSS-MRI组,50%患者行CAS,17%患者行CEA,术后一天弥散加权成像显示存在围手术期缺血性损伤(调整后优势比5.21;95%可信区间:2.78-9.79:P<0.0001)。然而,损伤的临床意义任然未知,因此,瑞士巴塞尔大学医院神经和卒中中心Henrik Gensicke博士等人对其进行了研究,成果发表在2月份Journal of the American College of Cardiology期刊上。
背景:颈动脉支架术(CAS)后,通过弥散加权成像(DWI)经常发现存在脑部损伤,但它们的临床相关性仍然未知。
目的:此研究旨在调查颈动脉支架术(CAS)或颈动脉内膜切除术(CEA)后围手术期缺血DWI损伤是否与复发脑血管事件升高有关。
方法:国际颈动脉支架研究(ICSS)亚组研究的磁共振成像(MRI)中,231例有症状的颈动脉狭窄患者随机接受CAS(N=124)或者CEA(N =107)。术前1-7天,治疗后1-3天进核磁共振成像。主要终点事件是术后进行MRI后和随访结束前,发生中风或短暂性脑缺血发作。CAS和CEA组术后扫描成像中,(DWI+)和(DWI-)患者新发DWI病损主要终点事件发生时间进行比较。
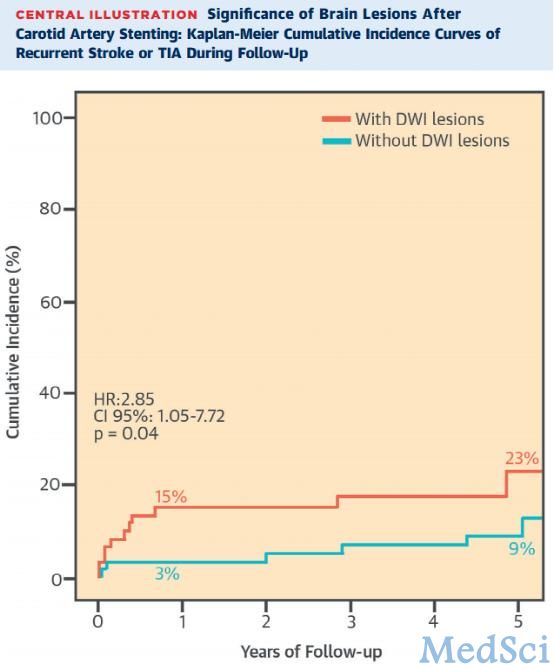
结果:随访中位时间为4.1年(四分位数间距:3.0〜5.2)。在CAS组,复发卒中或短暂性脑缺血发作DWI+患者(12/62例)比DWI-患者(6/62例)发生更频繁,累计5年发病率分别为22.8%(标准差:7.1%)和8.8%(标准差: 3.8%),未经调整的风险比:2.85;95%可信区间:1.05-7.72; P = 0.04)。在DWI+和DWI-患者,治疗6个月后,主要终点事件发生数分别为8和2。在CEA的组中,DWI+和DWI-患者复发脑血管事件没有差别。
结论:颈动脉支架术(CAS)后弥散加权成像(DWI)发现的缺血性脑损伤是复发脑血管事件风险升高的一个标志。患者围手术期DWI病损可能会受益于CAS术后积极长期的抗血小板治疗。(颈动脉支架术与颈动脉内膜剥脱术收益和成本效益的随机对比:国际颈动脉支架研究; ISRCTN25337470)。
原文出处:
Gensicke H, van der Worp HB, Nederkoorn PJ, et al. Ischemic brain lesions after carotid artery stenting increase future cerebrovascular risk. Journal of the American College of Cardiology. 2015;65(6):521-9.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支架术后#
24
#支架术#
20
#血管风险#
30
#JACC#
25
#颈动脉#
28
#颈动脉支架术#
24
#脑缺血损伤#
29
#颈动脉支架#
36
#脑缺血#
21
#ACC#
30