JAHA:房颤和利钠肽在预测心力衰竭住院或心血管死亡中的相互作用
2022-02-05 MedSci原创 MedSci原创
升高的NT-proBNP浓度可预测心房颤动患者未来的心力衰竭事件,无论是否伴有心力衰竭,这一结果鼓励在评估心房颤动患者时对NT-proBNP进行常规测量。
利钠肽常规测量主要用于心力衰竭诊断。它们的浓度在心房颤动患者中也会升高。

为了阐明它们在预测未来心血管事件中的价值,近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员测量了未选择的心血管疾病患者的利钠肽水平,并将它们的浓度与心房颤动和心力衰竭状态和结局进行关联分析。

研究人员将一家大型教学医院连续就诊的心血管疾病患者进行了临床评估、7天心电图监测和超声心动图检查,以诊断心房颤动和心力衰竭情况。研究人员集中测量了B型利钠肽前体N-末端(NT-proBNP)的浓度。根据回顾文献,研究人员根据浓度确定了四个NT-proBNP组(<300、300-999、1000-1999和≥2000pg/mL)。
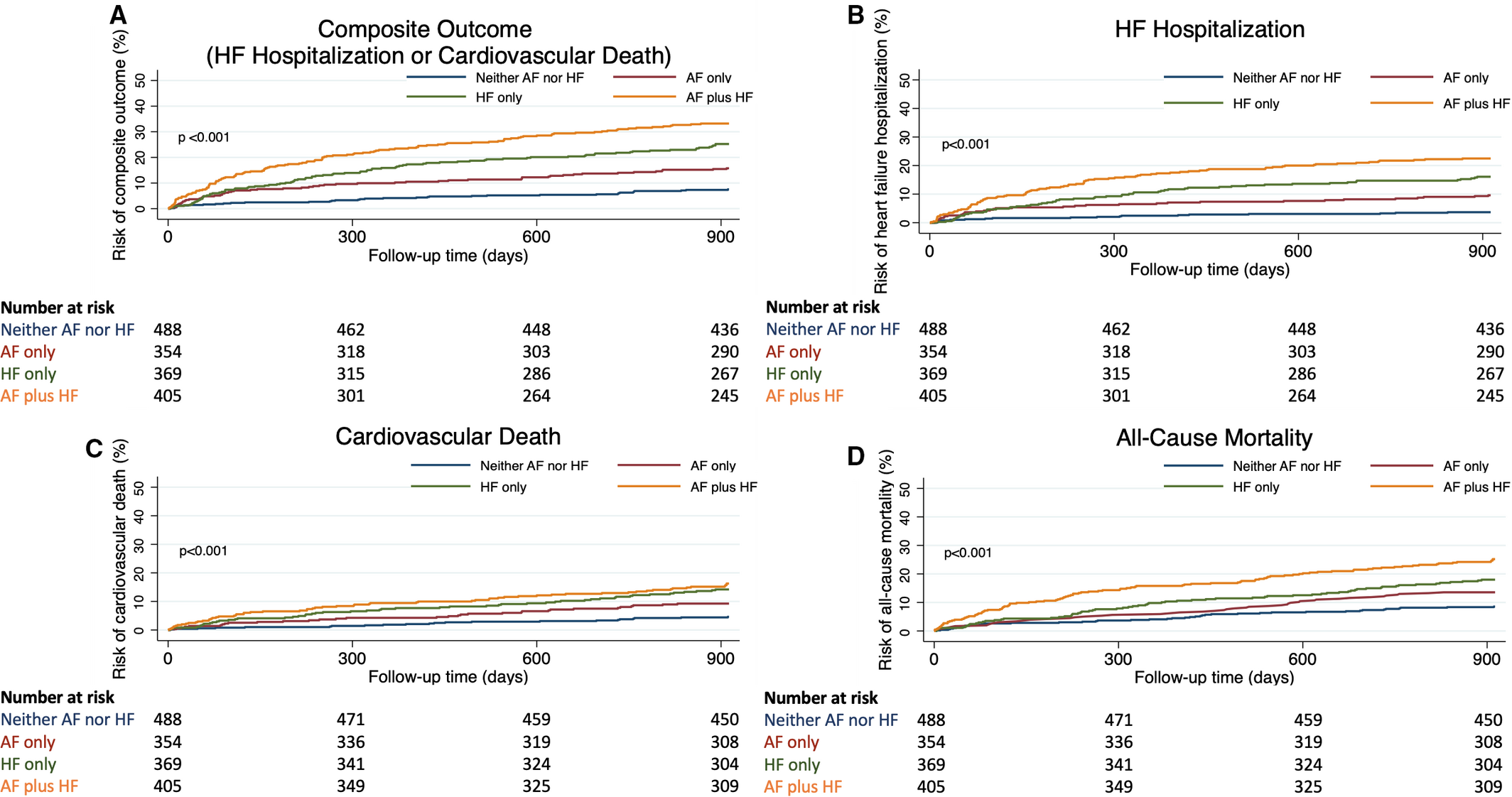
通过分析,研究人员发现临床特征和NT-proBNP浓度与心力衰竭住院或心血管死亡有关。1621名患者中有1616名(99.7%)人获得了随访数据,研究人员在对受试者进行了2.5年的随访后开展分析(中位年龄为70,[四分位距为60-78]岁;40%为女性)。心力衰竭住院或心血管死亡从488名在既没有心房颤动也没有心力衰竭的患者中的36人(3.2/100人/年)增加到354名仅为心房颤动患者中的55人(7.1/100人/年),在369名仅为心力衰竭患者中的92人(12.1/100人/年),405名心房颤动加心力衰竭患者中的128人(17.7/100人/年)(P<0.001)。较高的NT-proBNP浓度仅预测心房颤动患者(C统计量为0.82;95%CI为0.77-0.86;P<0.001)和其他表型患者(心房颤动加心力衰竭的C统计量为0.66;[95%CI为0.61–0.70];P<0.001)的结局。
由此可见,升高的NT-proBNP浓度可预测心房颤动患者未来的心力衰竭事件,无论是否伴有心力衰竭,这一结果鼓励在评估心房颤动患者时对NT-proBNP进行常规测量。
原始出处:
Paul F. Brady.et al.Interactions Between Atrial Fibrillation and Natriuretic Peptide in Predicting Heart Failure Hospitalization or Cardiovascular Death.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022833
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心力衰竭住院#
56
#相互作用#
57
好文😀
58
#AHA#
30
#利钠肽#
47
#互作#
39
#心血管死亡#
39