J Clin Oncol:依西美坦和恩替诺他联合治疗AI耐药的HR阳性、HER2阴性晚期乳腺癌
2021-08-08 Nebula MedSci原创
依西美坦和恩替诺他联合治疗AI耐药的HR阳性、HER2阴性晚期乳腺癌的疗效和安全性
晚期乳腺癌的内分泌治疗耐药仍然是一个重要的临床问题,可以通过组蛋白去乙酰化酶抑制剂(如,恩替诺特)克服。2期ENCORE301研究报告,在晚期激素受体 (HR) 阳性、人表皮生长因子受体2 (HER2) 阴性乳腺癌患者的在甾体芳香化酶抑制剂 (AI) 依西美坦中加入恩替他来可改善其无进展生存期 (PFS) 和总生存期 (OS)。
E2112: Randomized Phase III Trial of Endocrine Therapy Plus Entinostat or Placebo in Hormone Receptor-Positive Advanced Breast Cancer. A Trial of the ECOG-ACRIN Cancer Research Group
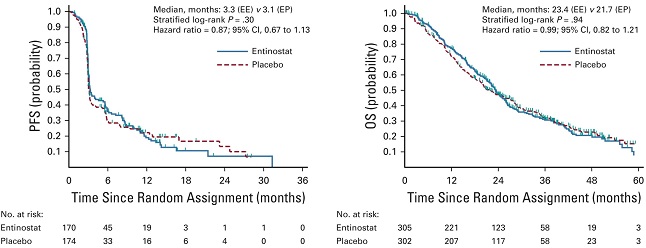
E2112研究是一项多中心、随机、双盲、安慰剂为对照的3期试验,招募了非甾体AI治疗后进展的HR阳性、HER2阴性的乳腺癌患者。受试患者被随机分成两组,接受依西美坦+恩替诺特(EE)或依西美坦+安慰剂(EP)治疗。主要终点是PFS和OS。次要终点包括安全性、客观缓解率和外周血单个核细胞的赖氨酸乙酰化变化。
在2014年3月至2018年10月期间,共有608位患者(中位年龄为 63岁,60%有内脏疾病,84%的患者经非甾体AI治疗后进展)随机分组。既往治疗包括化疗 (60%)、氟维司汀 (30%) 和周期素依赖性激酶抑制剂 (35%)。
两组的PFS和OS
EE组和EP组的中位PFS分别是3.3个月和3.1个月(风险比[HR] 0.87,p=0.30)。EE组和EP组的中位OS分别是23.4个月和21.7个月(HR 0.99;p=0.94)。EE组和EP组的客观缓解率分别为5.8%和5.6%。药效学分析证实了恩替诺特治疗患者的靶向抑制作用。
EE组的最常见的3/4级不良反应事件有中性粒细胞减少(20%)、低磷酸血症(14%)、贫血(8%)、白细胞减少(6%)、疲劳(4%)、腹泻(4%)和血小板减少(3%)。
很遗憾!该研究结果显示,依西美坦和恩替诺他联合治疗并没有提高AI耐药的HR阳性、HER2阴性的晚期乳腺癌患者的生存率。
原始出处:
Connolly Roisin M,Zhao Fengmin,Miller Kathy D et al. E2112: Randomized Phase III Trial of Endocrine Therapy Plus Entinostat or Placebo in Hormone Receptor-Positive Advanced Breast Cancer. A Trial of the ECOG-ACRIN Cancer Research Group.[J] .J Clin Oncol, 2021, undefined: JCO2100944.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#依西美坦#
34
#Oncol#
35
#HR阳性#
43
#联合治疗#
43
#HER2阴性#
42
谢谢梅斯分享这么多精彩信息
67
你好
64