Sci Rep:ESSIC 2型间质性膀胱炎/膀胱疼痛综合征和过度活跃膀胱中的尿液生物标志物与新的诊断算法开发
2021-02-15 AlexYang MedSci原创
最近,有研究人员调查了尿液细胞因子在间质性膀胱炎/膀胱疼痛综合征(IC/BPS)和过度活跃膀胱(OAB)的患者中的诊断价值,并开发一种新型诊断算法。
最近,有研究人员调查了尿液细胞因子在间质性膀胱炎/膀胱疼痛综合征(IC/BPS)和过度活跃膀胱(OAB)的患者中的诊断价值,并开发一种新型诊断算法。
研究人员共收集了40名IC/BPS和40名OAB患者以及30名对照组的尿液样本;并使用了商业化的多重免疫分析法分析了31种目标细胞因子。结果表明,研究组和对照组之间的尿液细胞因子情况有显著差异。MIP-1β显示出最高的灵敏度(92.2%),可以从对照组中识别患病的研究组患者。对区分IC和OAB具有较高诊断价值的细胞因子包括IL-10、RANTES、eotaxin、CXCL10、IL-12p70、NGF、IL-6、IL-17A、MCP-1和IL-1RA。随后研究人员根据得到的诊断值开发了诊断算法,并选择MIP-1β进行初筛测试来诊断疾病患者和对照组,其中诊断率分别为81.6%和68.4%。作为IC/BPS的确诊试验,eotaxin、CXCL10和RANTES的诊断率分别为73.3%、72.7%和69.7%。作为OAB的确诊试验,IL-10的诊断率为60%。
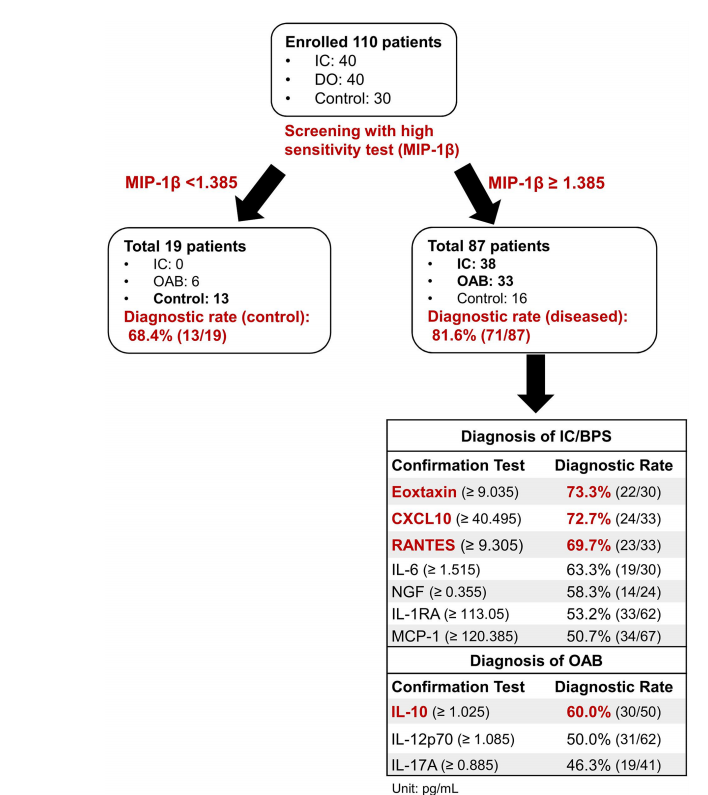
最后,研究人员指出,IC/BPS和OAB患者的尿液细胞因子谱与对照组不同,可能是诊断有用生物标志物。基于这些图谱,研究人员同时开发了一种新的试验性诊断算法。
原始出处:
Yuan-Hong Jiang, Jia-Fong Jhang, Yung-Hsiang Hsu et al. Urine biomarkers in ESSIC type 2 interstitial cystitis/bladder pain syndrome and overactive bladder with developing a novel diagnostic algorithm. Sci Rep. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SSI#
49
#间质性#
42
#过度活跃#
47
#标志物#
0
#间质性膀胱炎#
43
#综合征#
32
#尿液#
49
#生物标志#
31
#生物标志#
23