Ann Rheum Dis:替拉珠单抗治疗活动性银屑病关节炎的疗效和安全性——随机、双盲、安慰剂对照、多剂量、52周的IIb期研究结果
2021-10-18 MedSci原创 MedSci原创
银屑病关节炎(PsA)是一种慢性、进行性、炎症性的关节炎,估计全球患病率为0.2%-0.3%,为家庭和社会造成相当大的经济负担。近日,发表于Ann Rheum Dis的一项随机试验评估了抗白细胞介素-
银屑病关节炎(PsA)是一种慢性、进行性、炎症性的关节炎,估计全球患病率为0.2%-0.3%,为家庭和社会造成相当大的经济负担。近日,发表于Ann Rheum Dis的一项随机试验评估了抗白细胞介素-23p19单克隆抗体替拉珠单抗对银屑病关节炎(PsA)患者的疗效和安全性。
在这项随机、双盲、安慰剂对照的IIb期研究中,研究人员纳入了活动性PsA患者,按1:1:1:1的比例随机接受替拉珠单抗 200 mg,每4周一次(Q4W);替拉珠单抗 200、100或20 mg Q12W;或安慰剂Q4W。接受替拉珠单抗 20毫克或安慰剂的患者在W24时改用替拉珠单抗 200毫克Q12W;治疗持续到W52。主要疗效终点是在W24时发生ACR20反应(按美国风湿病学会标准改善≥20%)的患者比例。次要疗效终点的评估不需要对多重性进行校正。安全性是根据治疗中出现的不良事件(TEAEs)进行的评估。
结果,391/500名被筛选的患者接受了随机分组和治疗。在W24,替拉珠单抗治疗组71.4%-79.5%的患者与安慰剂组50.6%的患者达到ACR20(所有P<0.01)。与安慰剂组相比,替拉珠单抗治疗组患者在W24年和到W52年都能达到较高的ACR50、28个关节的疾病活动评分和C反应蛋白<3.2、最小疾病活动和比基线银屑病面积和严重程度指数改善75%/90%/100%的反应率。没有观察到腕关节炎和肌腱炎的改善;其他结果不一。在W24时改用替拉珠单抗 200 mg的患者的反应与基线的治疗一致。到W52,分别有64.5%和3.3%的患者发生TEAEs和严重TEAEs,各治疗组之间具有可比性。
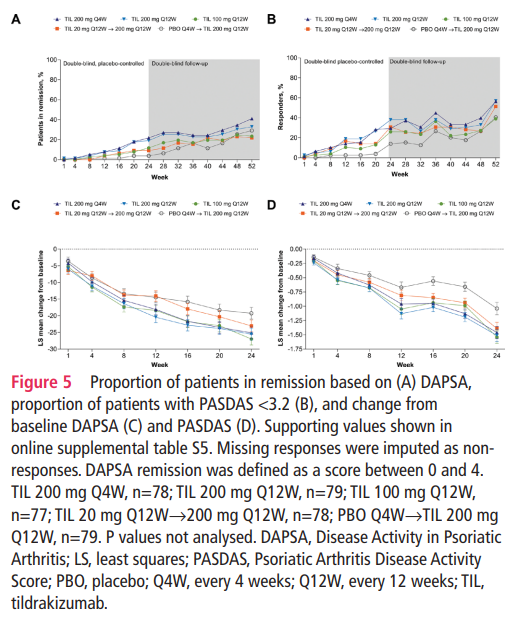
综上所述,该研究结果表明,替拉珠单抗治疗可明显改善PsA的关节和皮肤表现,但不包括腕关节炎和肌腱炎。到W52为止,治疗的耐受性普遍良好。
原始出处:
Philip J Mease, et al., Efficacy and safety of tildrakizumab in patients with active psoriatic arthritis: results of a randomised, double-blind, placebo-controlled, multiple-dose, 52-week phase IIb study. Ann Rheum Dis. 2021 Sep;80(9):1147-1157. doi: 10.1136/annrheumdis-2020-219014.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Dis#
47
#研究结果#
45
#活动性#
44
#对照#
49
#疗效和安全性#
38
#Ib期#
38
学习了
64
#关节炎#
22
#安慰剂#
38
#活动性银屑病关节炎#
44