J Rheumatol:粘膜相关恒定T细胞参与强直性脊柱炎的发病
2016-07-25 MedSci MedSci原创
来自日本内科和风湿病及免疫学组的研究人员发现粘膜相关的恒定T细胞可能在强直性脊柱炎中扮演了角色。 强直性脊柱炎(AS)是以外周关节和韧带附着点慢性炎症为主要症状的疾病。肠道免疫被认为与AS发病相关,因为在AS患者中观察到明显的肠道和关节炎症并存。粘膜免疫相关恒定T细胞(MAIT)倾向于定居在肠固有层并产生炎性细胞因子如白介素-17(IL-17)和肿瘤坏死因子-α (TNF-α),是AS的治疗
来自日本内科和风湿病及免疫学组的研究人员发现粘膜相关的恒定T细胞可能在强直性脊柱炎中扮演了角色。
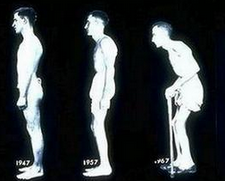
强直性脊柱炎(AS)是以外周关节和韧带附着点慢性炎症为主要症状的疾病。肠道免疫被认为与AS发病相关,因为在AS患者中观察到明显的肠道和关节炎症并存。粘膜免疫相关恒定T细胞(MAIT)倾向于定居在肠固有层并产生炎性细胞因子如白介素-17(IL-17)和肿瘤坏死因子-α (TNF-α),是AS的治疗目标。这个研究旨在调查MAIT细胞是如何参与AS的发病。
研究人员写道,"我们发现MAIT细胞在AS患中是激活的,但出现在外周血中的频率减少,尽管这次的研究表明MAIT细胞与AS发病相关。仍需进一步的研究确定MAIT细胞对疾病的发展和恶化的作用,以此更好的了解AS的发病机制。"
研究人员调查了30个AS患者和21个健康对照组中MAIT细胞出现的频率和细胞因子产物。使用流式细胞仪分析AS患者MAIT细胞激活标志物CD69。
研究发现,AS患者外周血中MAIT细胞出现的频率与健康对照组相比减少,有更高水平的MAIT细胞激活后产物白细胞介素-17,AS患者中强直性脊柱炎活动评分与MATI细胞CD69表达相关。
Hayashi E, et al. Involvement of Mucosal-associated Invariant T cells in Ankylosing Spondylitis,J Rheumatol. 2016; doi:10.3899/jrheum.151133
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#强直性#
25
好文章,受益
53
#粘膜#
29
赞了!深度好文,深入学习。
50
好文章,值得学习,先赞一个
51
#脊柱炎#
34
学习了,强直性脊柱炎越来越多发
77