女性,73岁,出现舌头右缘溃疡、白斑,以及吃东西时出现疼痛1年余。
既往无抽烟和饮酒史。
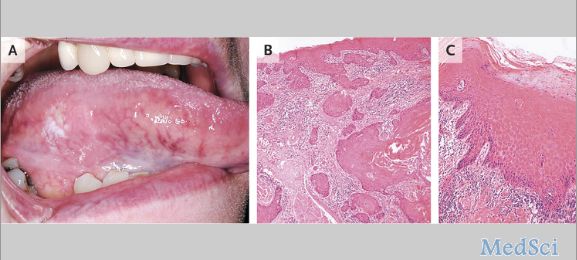
颈部淋巴结检查未触及肿大。口腔检查可见舌头浅表有一界限清楚,大小为7mmX3mm的溃疡。另外,在溃疡部位的边缘有硬化的现象,在舌头右缘的下边界有多处红白的斑点(如图A)。
硬结上缘切开取样活检显示浸润性鳞状细胞癌(如图B;苏木精伊红染色)。
斑点部位切开取样活检显示染色加深和多形性的基底上皮层细胞和“萌芽”结构,被视为轻度不典型增生(如图C;苏木精伊红染色)。
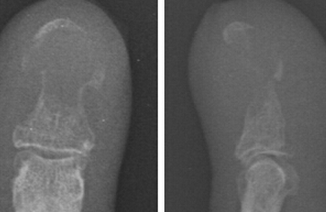
计算机断层扫描证实无颈部淋巴结受累。
最后,病人接受了癌变部位广泛性切除,在术后的12个月中,病人没有出现复发的现象。
目前,晚期的舌鳞状细胞癌患者,术后5年生存率仅仅保持在50%左右。在临床上,通常以取样活检为诊断的辅助手段,当活检结果显示细胞形状或结构改变时,高度怀疑癌变的可能。
原始出处:
Rui P.P. Albuquerque, D.D.S., Ph.D., and Andrea Richards, B.D.S., F.D.S. (Oral Med.) Squamous-Cell Carcinoma of the Tongue
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#舌鳞状细胞癌#
34
#细胞癌#
34
好文章,受益
89
好文章,还会关注
79
赞了!深度好文。
85
舌鳞癌,学习了
130