Diabetologia:糖皮质激素诱导的胰岛素抵抗降低肠促胰素效应
2015-04-02 沐晴 译 MedSci原创
最近,有研究评估了在健康个体使用糖皮质激素诱导胰岛素抵抗造成进展性T2DM模型,评估肠促胰素效应。试验中,挑选19名健康、糖耐量正常的T2DM一级亲属作为受试者。 在地塞米松治疗前,所有受试者都要进行第1天的OGTT试验,接着是为期3天葡萄糖钳夹试验,分别向受试者静注GLP-1、GIP或NaCl,最后静注精氨酸来明确胰岛beta细胞的最大分泌功能。地塞米松治疗5天后,重复这4天的试验。总
最近,有研究评估了在健康个体使用糖皮质激素诱导胰岛素抵抗造成进展性T2DM模型,评估肠促胰素效应。试验中,挑选19名健康、糖耐量正常的T2DM一级亲属作为受试者。
结果显示,在地塞米松治疗后,19名受试者胰岛素抵抗水平均升高了(评价指标:HOMA-IR胰岛素抵抗指数和胰岛素敏感指数,餐后2小时血糖浓度),然而,胰岛素beta细胞的分泌功能普遍升高了。在7mmol/l葡萄糖钳夹试验中,GLP-1和GIP诱导胰岛素反应,胰岛beta细胞最大分泌能力在两个阶段并无不同。然而,在第二阶段,7mmol/l葡萄糖钳夹试验,和第一阶段的15mmol/l葡萄糖钳夹试验,两种激素诱导的胰岛素反应均降低了。
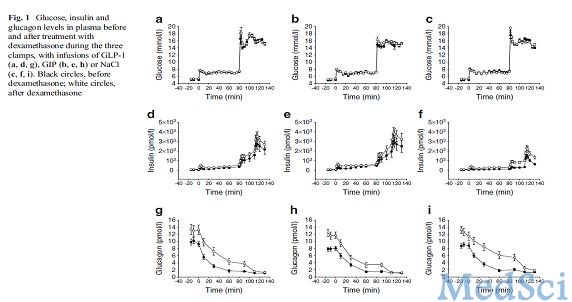
最后,研究者表示,在有发生T2DM风险的个体中,糖皮质激素诱导的胰岛素抵抗可以降低肠促胰素的促胰岛素分泌作用。这种肠促胰素效应的降低,与胰岛beta细胞的最大分泌能力降低无关,这表明在本试验中建立的进展性糖代谢紊乱模型中,肠促胰素效应降低是由于肠促胰素促胰素分泌作用本身的早期降低,并不是胰岛beta细胞功能受限所引起的。
注:葡萄糖钳夹技术是一种定量检测胰岛素分泌和胰岛素抵抗的方法。葡萄糖钳夹技术首先由Andres及其同事于1966年论述,被认为是现今最新的葡萄糖稳态的测量技术。钳夹试验已经成为评估和鉴别β细胞对于胰岛素反应敏感性的“金标准”方法。可分为高胰岛素-正常血糖钳夹和高葡萄糖变量钳夹。
Eriksen M, Jensen DH, Tribler S, Holst JJ, Madsbad S, Krarup T.Reduction of insulinotropic properties of GLP-1 and GIP after glucocorticoid-induced insulinresistance.Diabetologia. 2015 Mar 9. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
38
#DIA#
35
#胰岛#
37
好好学习一下
115
#肠促胰素#
35
#糖皮质#
32
AKI对心衰临床治疗意义重大,但依然需要研究检验其适用性
104
没明白
85
#皮质激素#
37
受教了
103