JAMA: 阿斯利康、杨森/强生COVID-19疫苗引起脑静脉窦血栓形成和血小板减少又添新佐证
2021-07-29 MedSci原创 MedSci原创
在新冠肺炎疫情前的脑静脉窦血栓患者中,基线血小板减少不常见,肝素诱导的血小板减少和血小板因子4/肝素抗体罕见
最近有报道称,在接种新冠肺炎疫苗ChAdOx1 nCov-19(阿斯利康/牛津)和AD26.CoV2.S(杨森/强生)后4至28天内,在不寻常部位发生血栓并伴有血小板减少的病例。许多报道的患者患有脑静脉窦血栓形成(CVST)。在几个欧洲国家暂停接种ChAdOx1 nCov-19疫苗后,在欧洲药品管理局进行了效益和风险评估后,大多数这些国家恢复了疫苗接种,但仅限于较老的年龄组。在美国,根据食品药品监督管理局和疾病控制和预防中心的建议,暂停接种AD26.CoV2.S疫苗后,恢复了疫苗接种。与血小板4因子/肝素抗体相关的免疫介导反应被认为是潜在的病理机制。
Mayte Sánchez van Kammen等探讨了新冠肺炎疫情前脑静脉窦血栓形成患者入院血小板减少、肝素诱导的血小板减少和血小板因子4/肝素抗体的发生率。研究结果发表在JAMA杂志。


在952例患者中,865例有可用的基线血小板计数。在93名患者的子集中,分析了一项研究在2009年9月至2016年2月的收集的冰冻血浆样本是否存在血小板因子4/肝素抗体。
主要观察指标为入院血小板减少(血小板计数<150×103/μL)、肝素诱导的血小板减少(由治疗医生诊断)和血小板因子4/肝素IgG抗体(光密度>0.4,在以前收集的血浆样本的一组患者中)的频率。
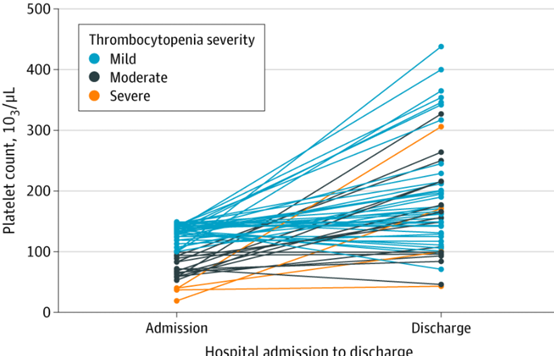
56例脑静脉窦血栓形成伴血小板减少患者入院及出院时血小板计数
865例患者(中位年龄40岁[四分位数间范围29~53岁],70%为女性)中,血小板减少73例(8.4%;95%CI,6.8%~10.5%),轻度(100~149×103/μL)52例(6.0%),中度(50~99×103/μL)17例(2.0%),重度(<50×103/μL)4例(0.5%)。肝素诱导的血小板减少并血小板因子4/肝素抗体在单个患者中被诊断为(0.1%;95%CI,<0.1%-0.7%)。在实验室分析的93例脑静脉窦血栓患者中,8例(9%)有血小板减少,无一例(95%CI,0%-4%)有血小板因子4/肝素抗体。
这项研究中,865名COVID-19大流行前CVST患者出现血小板减少时并不常见。在许多患者中,血小板减少症可以解释为合并症,如癌症或感染,或使用酒精或某些药物。只有1例患者确诊为HIT。由于CVST患者没有进行HIT常规筛查,从93名患者中抽取额外的血浆样本进行PF4/肝素抗体检测,没有一个阳性检测结果。
在新冠肺炎疫情前的脑静脉窦血栓患者中,基线血小板减少不常见,肝素诱导的血小板减少和血小板因子4/肝素抗体罕见。这些发现可能有助于研究ChAdOx1 nCoV-19和AD26.CoV2.S COVID-19疫苗与脑静脉窦血栓形成和血小板减少之间的可能联系。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
42
#静脉窦血栓#
49
#强生#
56
#血小板减少#
44
#杨森#
44
#静脉窦#
32
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
59