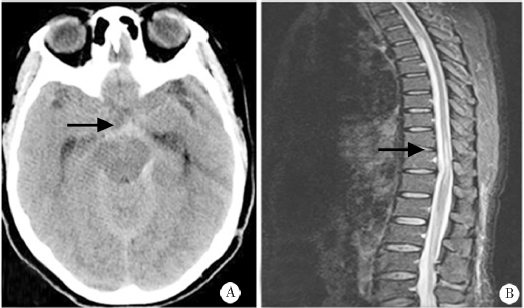
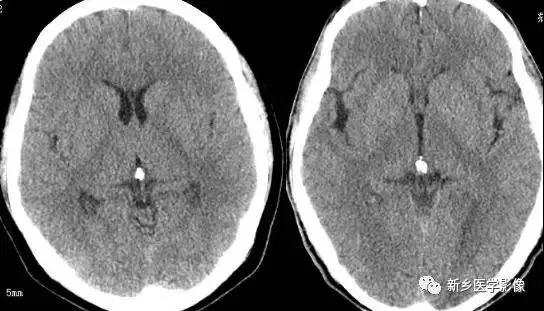
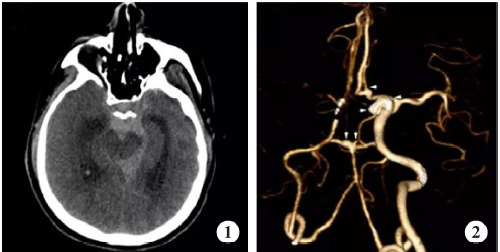
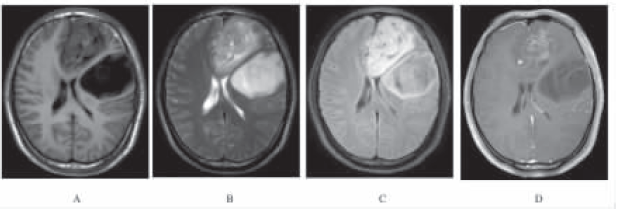
以颅内蛛网膜下腔出血为表现的脊髓硬脊膜动静脉瘘4例
2019-03-30 高俊华 李务荣 郑博文 疑难病杂志
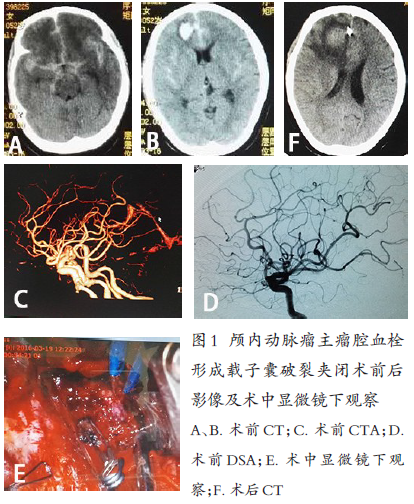
2011年8月—2016年10月首都医科大学附属北京地坛医院神经内科确诊颅内SAH患者4例,经全脑或脊髓(digital subtraction angiography,DSA)观察到硬脊膜处供血动脉与引流静脉形成的瘘口确诊SDAVF。男3例,女1例,年龄48~58岁,中位年龄53岁。确诊时间在发病后1~8d。既往曾有一次剧烈头痛伴呕吐患者1例,未诊治,自行好转。余患者既往体健。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#脊髓硬脊膜#
42
#蛛网膜#
37
#静脉#
44
#动静脉瘘#
55
#硬脊膜#
42