J Stroke Cerebrovasc Dis:血浆免疫蛋白体升高可预测急性缺血性卒中早期出血转化
2016-10-25 MedSci MedSci原创
背景:目前血液生物标志物与出血性转化(HT)增加的相关性的风险仍不确定。研究者旨在确定免疫蛋白酶体作为预测急性缺血性脑卒中患者早期HT的意义。方法:这项研究纳入了316例缺血性卒中患者。在卒中后5±2天或临床上恶化(CD)后行CT检查评估HT。应用定量夹心酶联免疫吸附测定试剂盒测定LMP2、MECL-1、白细胞介素-1 LMP7,IL-1β和超敏C反应蛋白(hs-CRP)。应用多元Logistic
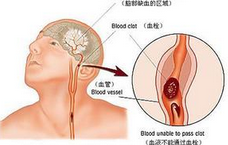
背景:目前血液生物标志物与出血性转化(HT)增加的相关性的风险仍不确定。研究者旨在确定免疫蛋白酶体作为预测急性缺血性脑卒中患者早期HT的意义。
方法:这项研究纳入了316例缺血性卒中患者。在卒中后5±2天或临床上恶化(CD)后行CT检查评估HT。应用定量夹心酶联免疫吸附测定试剂盒测定LMP2、MECL-1、白细胞介素-1 LMP7,IL-1β和超敏C反应蛋白(hs-CRP)。应用多元Logistic回归分析与HT相关的因素。
结果:有42(13.3%,42/316)发生了HT患者。与无HT患者相比,有出血性转化的患者入院血浆LMP2、MECL-1、LMP7,IL1-β,和hs-CRP浓度明显升高。这些蛋白质浓度增加与出血的严重程度相关。CD的HT患者LMP2的最高水平(1679.5 [ 1394.6-136.6 ] pg/ml),MECL-1(992.5 [ 849.7-1075.8 ] pg/ml),LMP7(822.6 [ 748.6-1009.5 ] pg/ml),IL-1β(113.2 [ 90.6-194.5 ] pg/ml)及hs-CRP(30 [ 12.8-75.6 ] mg/L)。Logistic回归分析显示,心源性脑栓塞、LMP2、MECL-1和LMP7为HT的独立预测因子。ROC曲线分析显示LMP2 ≥ 988.3 pg/ml,MECL-1 ≥ 584.7 pg/ml,LMP7≥ 509 pg/ml是HT的独立因素。
结论:血浆免疫蛋白酶体可有助于预测急性缺血性卒中患者的早期HT。
原始出处:
Chen X, Wang Y,et al. Plasma Immunoproteasome Predicts Early Hemorrhagic Transformation in Acute Ischemic Stroke Patients. J Stroke Cerebrovasc Dis. 2016 Sep 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#缺血性卒#
24
#Dis#
22
#缺血性#
21
#ASC#
21
学习了,再关注一下
54