Blood:多发性骨髓瘤亚克隆的TP53拷贝数可独立指示患者预后
2018-11-02 MedSci MedSci原创
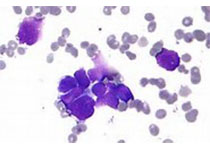
中心点:在新确诊的多发性骨髓瘤中,微小肿瘤亚克隆的TP53缺失是独立的预后因素。采用MLPA评估肿瘤亚克隆的TP53缺失,可用于标准诊断,有助于对患者进行分层管理。摘要:多发性骨髓瘤(MM)是一种遗传性的骨髓浆细胞异质性肿瘤,预后不一。为评估TP53拷贝数克隆异质性的预后相关性,Vallari Shah等人采用多重结扎依赖性探针扩增(MLPA)对骨髓瘤XI试验的1777例新确诊的骨髓瘤患者的肿瘤进
在新确诊的多发性骨髓瘤中,微小肿瘤亚克隆的TP53缺失是独立的预后因素。
摘要:
多发性骨髓瘤(MM)是一种遗传性的骨髓浆细胞异质性肿瘤,预后不一。为评估TP53拷贝数克隆异质性的预后相关性,Vallari Shah等人采用多重结扎依赖性探针扩增(MLPA)对骨髓瘤XI试验的1777例新确诊的骨髓瘤患者的肿瘤进行异质性分析。
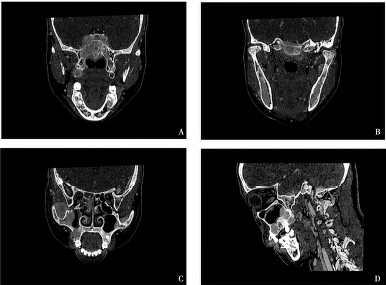
亚克隆TP53缺失与总体存活期更短独立相关,风险比高达1.8(95% CI 1.2-2.8;p=0.01)。克隆的(非亚克隆)TP53缺失与晚期病程的临床标志物相关,特别是血小板计数降低(p<0.001)、LDH(乳酸脱氢酶)升高(p<0.001)和指示基因组不稳定del(13q)或del(1p)的特征频率增高(p=0.002、p=0.006)。突变和缺失导致TP53双等位基因丧失功能的概率非常低(2.4%),与晚期疾病密切相关。
通过MLPA识别肿瘤亚克隆是否存在TP53缺失,或可改善多发性骨髓瘤患者的分层管理,促进个体化治疗。
Vallari Shah,et al. Sub-clonal TP53 copy number is associated with prognosis in multiple myeloma. Blood 2018 :blood-2018-06-857250; doi: https://doi.org/10.1182/blood-2018-06-857250
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#克隆#
34
#患者预后#
37
#拷贝数#
38
#多发性#
44
#亚克隆#
39
#p53#
33
#TP53#
38
了解一下,谢谢分享!
79