Nature:外泌体可能是癌症播散真正的种子
2015-10-30 何嫱 译 生物通
了解肿瘤转移至一种特定器官而不去到其他器官处的原因是肿瘤学的首要目标之一,也是最古老的目标之一。126年前,英国医生Stephen Paget阐述了他的“种子与土壤理论”,主张转移需要肿瘤细胞传播即“种子”,和受纳器官理想的环境即“肥沃的土壤”。然而,自那时以后在阐析引导癌症转移至特异器官的机制方面一直未取得极大的进展。 近来,西班牙国家癌症中心(CNIO)微环境和癌症转移小组组长H
了解肿瘤转移至一种特定器官而不去到其他器官处的原因是肿瘤学的首要目标之一,也是最古老的目标之一。126年前,英国医生Stephen Paget阐述了他的“种子与土壤理论”,主张转移需要肿瘤细胞传播即“种子”,和受纳器官理想的环境即“肥沃的土壤”。然而,自那时以后在阐析引导癌症转移至特异器官的机制方面一直未取得极大的进展。
近来,西班牙国家癌症中心(CNIO)微环境和癌症转移小组组长Héctor Peinado,威尔康乃尔医学院的David Lyden,和纪念斯隆凯特琳癌症中心的Jaqueline Bromberg,发展出了一套理论来支持Paget的“种子与土壤”学说。
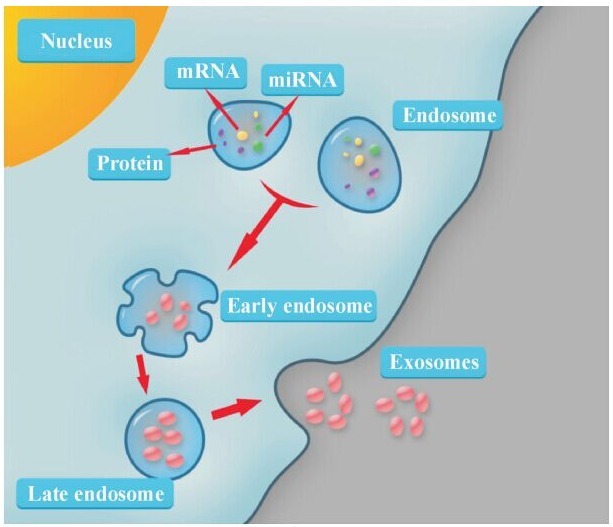
在发表于《自然》(Nature)杂志上的一篇论文中,共同第一作者Ayuko Hoshino、Bruno Costa-Silva与Peinado和Lyden一起收集了证据证实,肿瘤释放了数百万携带着它们的蛋白质和遗传内容物的囊泡。这些囊泡叫做外泌体(exosome),像“通信船”或“侦察舰”一样,它们确保了受纳器官做好准备招待肿瘤细胞。具体说来,外泌体触发了受纳器官中必要的分子反应——炎症、血管形成等来欢迎肿瘤细胞,使得当肿瘤细胞到达时可以进行增殖。该团队在今年夏天在Nature Cell biology上发表文章发现胰腺癌首先通过外泌体在肝脏埋下种子。
Peinado说:“到目前为止,这是第一项研究定义肿瘤分泌的外泌体在器官特异性转移中所起的作用。”当前的研究确证了存在外泌体,它证实外泌体在精确器官形成转移灶中发挥了至关重要的作用。
但研究人员想走得更远。他们知道在数百万源自肿瘤的外泌体中,只有少数将会筑巢,并且它们不会在随机的器官中这样做,而是优先选择一些器官。原因为何?是否有可能因为肿瘤的“侦察舰”外泌体具有一些分子标记,以某种方式引导了它们去到特定的器官?
外泌体中的“邮政编码”
为了验证这一假说,作者们选择了来自大约十种不同肿瘤的20个肿瘤细胞系,已知其中的一些肿瘤转移至特定靶器官:肺脏、肝脏、大脑或骨骼。他们分析了肿瘤外泌体中的近1000种蛋白,搜寻了那些发挥邮政编码作用的蛋白质。
他们将焦点放在了整合素(integrin)的蛋白质家族上,蛋白质组学研究显示,在肺转移中外泌体integrins α6β4 和 α6β1起关键作用。而外泌体中 integrin αvβ5 在肝转移中起关键作用。如果下调integrins α6β4 和αvβ5,能分别阻止肝肺转移。这些蛋白存在于外泌体膜上——理论上,目的地“标记”应该存在于这里。这被证实是一种很好地策略。从一千多种蛋白质中,他们发现了确实有一个特异的整合素组合与转移至肺脏及转移至肝脏相关。
Peinado指出:“我们已经确定了在肿瘤外泌体中有一个整合素组合使得在不同的器官,尤其是在肺脏和肝脏中易于形成转移微环境。我们的研究表明,在外泌体表面有一种‘邮政编码’使得它们去到了特定器官进行累积,在那里将会发生转移。”
如果通过改变目的地编码来“欺骗”肿瘤,它将会移植到指定的器官。采用正常去到骨骼的肿瘤细胞对此进行测试,在研究人员进行干预后,最终细胞去到了肺脏。这些数据支持了在转移过程中“土壤”和“种子”一样重要。
整合素在转移筑巢中起重要作用的另一个证据是,研究证实在转移至特定器官的肿瘤(例如,乳腺癌转移至肺脏,胰腺癌转移至肝脏)中阻断特异的整合素,可减少这些器官中的癌症转移。
奠定基础
研究人员还发现了当外泌体到达时调节受纳组织反应的分子信号。具体说来,这些信号与S100家族基因增加有关,众所周知这会引发炎症反应;炎症是一种与癌症相关的过程。
这些结果鉴别出了一些新的潜在药物靶点。Peinado说:“我们确定了癌症转移至特定器官的一种新机制,其与整合素及S100蛋白相关,可以利用它们来作为对抗癌症转移的新靶点。”
Peinado说:“我们的工作表明,在乳腺癌和胰腺癌患者血浆中某些整合素高水平表达,似乎预测了将会发生转移的器官。不过必须要在更大的群体研究中来验证这些数据及开发出一些预测测试。”
这些研究结果为研究人员生成了一个近期任务列表,从扩大患者研究以提高整合素的预测能力,到鉴别决定转移至大脑或骨骼的其他“邮政编码”。
同样重要的还有寻找新药物:“在未来,我们设想要开发出一些分子来特异地阻断肿瘤组织中的整合素组合,”Peinado说。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
36
这篇文章有一定深度
162
是一篇不错的文章
121
受教了。
128
厉害
152
MedSci上信息总令人脑洞大开
141
很有想法,值得借鉴
50