Blood:IGF-1通过激活Akt促进血小板生成
2018-05-27 MedSci MedSci原创
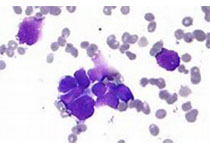
中心点:IGF-1可促进MK分化、形成血小板前体以及血小板释放。IGF-1对血栓形成的影响主要受SRC-3协助AKT激活所介导。摘要:众所周知,胰岛素样生长因子-1(IGF-1)还可作为造血生长因子,但其对血栓形成的直接作用尚不清楚。近日,Blood杂志上发表一篇文章,Shilei Chen等人发现IGF-1可促进CD34+细胞分化成巨核细胞(MKs),并能促进体外培养的MKs细胞形成血小板前体(
IGF-1可促进MK分化、形成血小板前体以及血小板释放。
IGF-1对血栓形成的影响主要受SRC-3协助AKT激活所介导。
摘要:
众所周知,胰岛素样生长因子-1(IGF-1)还可作为造血生长因子,但其对血栓形成的直接作用尚不清楚。近日,Blood杂志上发表一篇文章,Shilei Chen等人发现IGF-1可促进CD34+细胞分化成巨核细胞(MKs),并能促进体外培养的MKs细胞形成血小板前体(PPF)和血小板。研究人员同时用体内研究证实给放射(6.0Gy)处理过的和致命性放射(10.0Gy)后进行骨髓移植(BMT)的小鼠注射IGF-1可促进其血小板恢复。
深入研究发现ERK1/2和Akt激活介导IGF-1对血小板形成的作用。而且,与用促血小板生成素(TPO)处理所诱导的效应相比,IGF-1所诱导Akt激活明显高于ERK1/2激活。此外,IGF-1治疗还可显著增加TPO受体纯合突变小鼠的血小板计数,因此研究人员推测IGF-1对血小板形成的效应不依赖于TPO信号,进一步研究显示IGF-1触发的Akt激活需要类固醇受体共激活剂-3(SRC-3)辅助。
原始出处:
Shilei Chen,et al. IGF-1 facilitates thrombopoiesis primarily through Akt activation. Blood 2018 :blood-2018-01-825927; doi: https://doi.org/10.1182/blood-2018-01-825927
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#IGF#
60
#Akt#
36
#IGF-1#
29
学习了谢谢
70
谢谢分享
50
vvv刚刚好哈哈哈
45