J CEREBR BLOOD F M:脑脊液血红蛋白促进蛛网膜下腔出血相关的继发性脑损伤
2021-06-22 MedSci原创 MedSci原创
高CSF-Hb水平与SAH-SBI之间存在临床关联,在体外实验中,结合珠蛋白和血红素结合蛋白的益处使CSF-Hb成为SAH-SBI治疗极具吸引力的生物标志物和潜在的药物靶点。
动脉瘤性蛛网膜下腔出血 (SAH-SBI) 后继发性脑损伤导致颅内动脉瘤破裂后患者的预后不良。
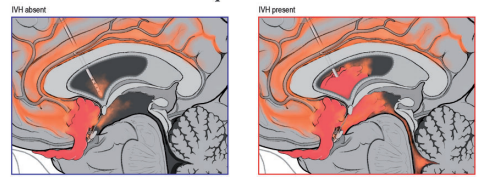
近日,脑血管和代谢疾病权威杂志Journal of Cerebral Blood Flow & Metabolism上发表了一篇研究文章,该研究旨在调查脑脊液中血红蛋白(CSF-Hb)和SAH-SBI之间的临床和病理生理学关联。
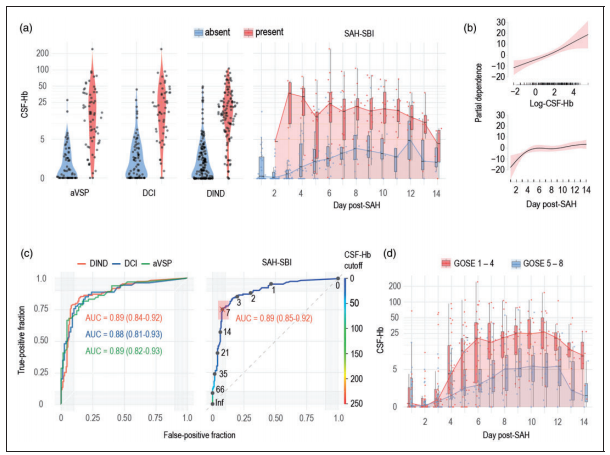
在47名患者的队列中,研究人员在动脉瘤破裂后的14天内每天收集CSF样本。
 动脉瘤性蛛网膜下腔出血后脑脊液血红蛋白与继发性脑损伤的关系
动脉瘤性蛛网膜下腔出血后脑脊液血红蛋白与继发性脑损伤的关系
有非常有力的证据表明分光光度法测定的CSF-Hb和SAH-SBI之间存在正相关。CSF-Hb监测SAH-SBI的准确性明显超过既定方法(AUC:0.89[0.85-0.92])。时间蛋白质组分析显示红细胞溶解伴随着适应性巨噬细胞反应,这是动脉瘤破裂后脑脊液中的两个主要生物过程。对Hb的血管收缩和氧化能力的体外实验揭示了SAH-SBI患者中与CSF-Hb阈值重叠的关键拐点。结合珠蛋白或血红素结合蛋白的选择性消耗和中和有效地减弱了CSF-Hb的血管收缩和脂质过氧化活性。
总的来说,高CSF-Hb水平与SAH-SBI之间存在临床关联,在体外实验中,结合珠蛋白和血红素结合蛋白的益处使CSF-Hb成为SAH-SBI治疗极具吸引力的生物标志物和潜在的药物靶点。
原始出处:
Kevin Akeret.et al.Cerebrospinal fluid hemoglobin drives subarachnoid hemorrhage-related secondary brain injury.Journal of Cerebral Blood Flow & Metabolism.2021.https://journals.sagepub.com/doi/full/10.1177/0271678X211020629
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#蛛网膜#
36
#继发#
25
#继发性#
48
#损伤#
25
学习了,不错。
53