JCE:ICD可用于预防心脏病瓣膜病患者的心脏病猝死
2012-12-28 JCE 互联网 czs890510
据统计,在美国每年有40万人死于心脏性猝死(SCD),其中心脏瓣膜病是导致SCD的第四位原因,前三位原因是冠心病、原发性心肌病和心脏传导障碍。左室收缩功能障碍是心脏性猝死的主要危险因素,心脏瓣膜病患者在换瓣术后持续的左室收缩功能障碍显着增加了SCD发生的机会。 既往多项临床研究表明,植入式心脏转复除颤器(ICD)可有效地用于缺血性心肌病和扩张型心肌病患者SCD的一级和二级预防,然而这些大规模的临
据统计,在美国每年有40万人死于心脏性猝死(SCD),其中心脏瓣膜病是导致SCD的第四位原因,前三位原因是冠心病、原发性心肌病和心脏传导障碍。左室收缩功能障碍是心脏性猝死的主要危险因素,心脏瓣膜病患者在换瓣术后持续的左室收缩功能障碍显着增加了SCD发生的机会。
既往多项临床研究表明,植入式心脏转复除颤器(ICD)可有效地用于缺血性心肌病和扩张型心肌病患者SCD的一级和二级预防,然而这些大规模的临床研究往往将瓣膜性心脏病患者排除,因此ICD是否能预防单个瓣膜或多个瓣膜性心脏病患者SCD的发生目前还不清楚,我们推测瓣膜性心脏病患者植入ICD后的死亡率及正确放电率与缺血性心肌病和扩张型心肌病相似。据此,Valles AG等进行了一项临床研究,旨在证实ICD植入对瓣膜性心脏病患者同样具有预防SCD的作用。
该研究入选的研究组为心脏瓣膜病换瓣术后植入ICD的患者,对照组为年龄、性别相匹配的植入ICD的缺血性心肌病或扩张型心肌病患者;另一个对照组则是瓣膜性心脏病患者进行过换瓣术,而未植入ICD患者。该研究主要比较研究组和对照组的死亡率和正确放电率。
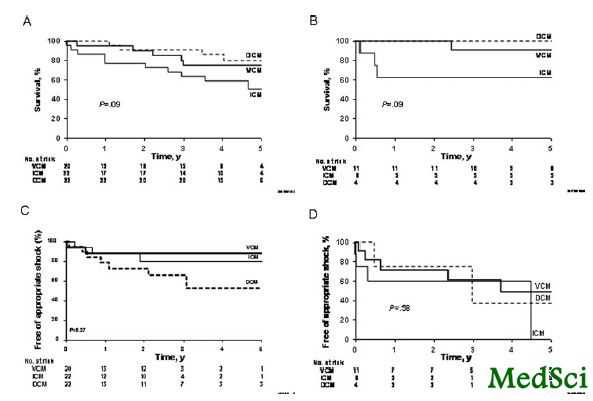
结果提示:研究组共入选31例患者,对照组中,30例为缺血性心肌病植入ICD患者,26例为扩张型心肌病植入ICD患者,62例为瓣膜性心脏病未植入ICD患者,所有患者的平均年龄为60岁,其中73%的患者为男性。对于植入ICD的患者,瓣膜性心脏病、缺血性心肌病及扩张型心肌病的平均LVEF值分别为34%、26%和23%。通过平均4.1年的随访,植入ICD患者中,三组的死亡率无明显差异,三组的正确放电率为5%、10%和4%。相比于未植入ICD的瓣膜性心脏病患者,植入ICD的患者死亡率为明显差异。
通过该项研究可得出以下结论:瓣膜性心脏病患者植入ICD预防SCD与扩张型心肌病和缺血性心肌病相比,具有类似的死亡率和正确放电率。该项研究结果还需要更大规模的临床研究来验证。

DOI: 10.1111/j.1540-8167.2012.02394.x
PMC:
PMID:
Implantable Cardioverter Defibrillators in Patients with Valvular Cardiomyopathy
ALFRED G. VALLES M.D.1, FARHAN J. KHAWAJA M.D.2, BERNARD J. GERSH M.B., Ch.B., D.Phil.1, MAURICE ENRIQUEZ-SARANO M.D.1, PAUL A. FRIEDMAN M.D.1, SOON J. PARK M.D.3, DAVID O. HODGE M.S.4, YONG-MEI CHA M.D.1
Sudden Death Prevention in Valvular Cardiomyopathy. Background: Implantable cardioverter-defibrillators (ICDs) are beneficial for preventing sudden cardiac death (SCD) in patients with previous SCD or left ventricular dysfunction. Objective: The objective was to investigate the outcomes of ICD implantation in patients who have surgery for valvular cardiomyopathy (VCM). Methods: We identified patients with VCM who had ICD implantation after valve surgery. Age- and sex-matched patients who received an ICD for ischemic cardiomyopathy (ICM) and dilated cardiomyopathy (DCM) served as controls. Patients with VCM who had valve surgery but did not receive an ICD served as an additional control group. We compared mortality and appropriate ICD discharges between the study group and control groups. Results: Mean (SD) age (31 patients with VCM with ICD, 30 with ICM, 26 with DCM, and 62 patients with VCM without ICD) was 60 (15) years, 73% were men. Ejection fraction at ICD implantation was 34%, 26%, and 23% for the VCM with ICD, ICM, and DCM groups, respectively (P = 0.03). After a median follow-up of 4.1 years, survival was not significantly different among ICD groups (P = 0.06). The annual appropriate shock rate was 5%, 10%, and 4% for the VCM with ICD, ICM, and DCM groups, respectively (P = 0.71). Compared to VCM without ICD, patients with VCM and ICD had comparable survival (P = 0.82) despite a reduced LVEF following valve surgery. Conclusion: Patients with VCM who undergo ICD implantation for SCD prevention have similar appropriate ICD discharge rates and mortality as do those with ICM and DCM. These data are hypothesis generating and deserve confirmation with large-scale prospective studies
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JCE#
40
#ICD#
32
#瓣膜#
38