Heart Rhythm:不同新型起搏技术的心室除极差异
2021-05-02 Nebula MedSci原创
nsLBBp保留了生理性左心室除极,但增加了心室间电不同步性。LVSP期间LV侧壁去极化时间延长,但心室同步性得以维持
近年来,出现了新的起搏技术,如His-Purkinje传导系统起搏。除了His束起搏(HBp)之外,此外,还有使用跨中隔方法对左心室间隔心肌起搏(LVSP)以及对左Tawara束的直接捕获(LBBp)。
非选择性His束起搏术(nsHBp)、非选择性左束支起搏术(nsLBBp)和左心室间隔心肌起搏(LVSP)是公认的生理性起搏技术,但这些起搏术的具体差异尚未有明确的定论。
本研究旨在采用两种超高频心电图(UHF-ECG)比较这些技术进行心室除极的差异。
招募了心动过缓患者,予以了nsHBp、nsLBBp(确认伴发LBB和心肌俘获)或LVSP(未证实LBB俘获的LV间隔位起搏)。用UHF-ECG显示心前导联的心室激动时间,并计算电子不同步e-DYS作为第一次激活与最后一次激活之间的差。以UHF-QRS复合波振幅50%的宽度来确定局部去极化(Vd)的持续时间。
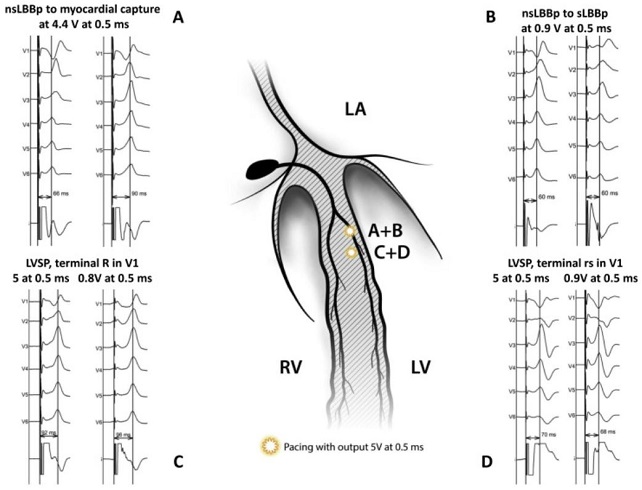
不同起搏术示意图
共68例患者,分别接受了nsLBBp(35例)、LVSP(96例)或nsHBp(55例)治疗,并在治疗期间收集了相应的数据。nsLBBp的e-DSY大于LVSP和nsHBp,分别为:-24 ms vs -12 ms vs 10 ms(p<0.001)。nsLBBp在V5-V8导联上的Vd值与nsHBp的相似(36-43 ms vs 38-43 ms),但在V1-V4导联上的Vd值比nsHBp的长(47-59 ms vs 41-44 ms,p<0.05)。LVSP使V1-V8导联上的Vd值较nsHBp的延长,V5-V8导联的Vd值也较nsLBBp的延长(44-51 ms vs 36-43 ms,p<0.05),且无论V5导联的R波峰时或V1导联QRS形态如何。
综上所述,nsLBBp保留了生理性左心室除极,但增加了心室间电不同步性。LVSP期间LV侧壁去极化时间延长,但心室同步性得以维持。
原始出处:
Curila Karol,Jurak Pavel,Jastrzebski Marek et al. The left bundle branch pacing compared to left ventricular septal myocardial pacing increases interventricular dyssynchrony but accelerates left ventricular lateral wall depolarization. Heart Rhythm, 2021, https://doi.org/10.1016/j.hrthm.2021.04.025
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











🐂
52
#ART#
35
#HEART#
27
🤙🤙🤙
65