Diabetologia:IGFBP-1在人2型糖尿病肾小球中的表达降低并调节人足细胞中的β1-整联蛋白/FAK信号传导
2021-09-30 从医路漫漫 MedSci原创
足细胞丢失或损伤是糖尿病肾病(DKD)发病机制中观察到的最早的特征之一,这是全球终末期肾衰竭的主要原因。胰岛素样生长因子轴功能障碍,包括胰岛素样生长因子结合蛋白(IGFBPs),与DKD有关
目的:足细胞丢失或损伤是糖尿病肾病(DKD)发病机制中观察到的最早的特征之一,这是全球终末期肾衰竭的主要原因。胰岛素样生长因子轴功能障碍,包括胰岛素样生长因子结合蛋白(IGFBPs),与DKD有关,特别是在疾病进展的早期阶段。这项研究的目的是研究IGFBPs在2型DKD发生中的潜在作用,重点是足细胞。
方法:分析IGFBP在PIMA DKD队列中的表达,以及来自Nephroseq数据库的数据,以及体外人肾小球中的IGFBP表达。体外研究了人足细胞和肾小球内皮细胞,用定量PCR和ELISA分析IGFBP-1的表达。细胞对IGFBPs的反应通过迁移、细胞存活和粘附分析、细胞-底物阻抗传感、Western blotting和高含量自动成像来研究。
结果:来自PIMA DKD队列和Nephroseq数据库的数据显示,在人类2型DKD的早期阶段,肾小球IGFBP-1显著减少。在肾小球中,IGFBP-1主要表达于足细胞,并受磷脂酰肌醇3-激酶(PI3K)-叉头盒O1(FoxO1)活性控制。在体外,IGFBP1通过β1整合素向足细胞发出信号,导致粘着斑激酶磷酸化,增加足细胞的运动性、粘附性、跨粘附细胞层的电阻和细胞存活率。
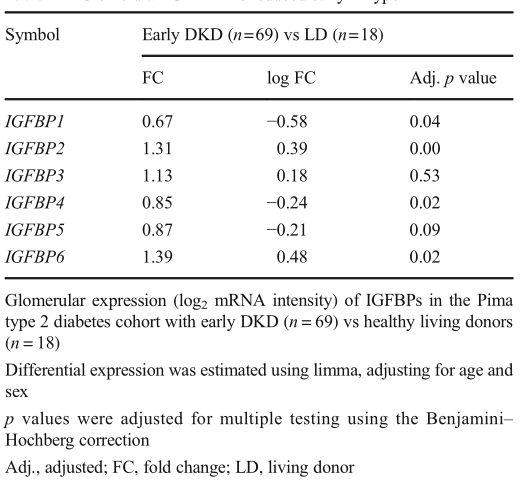
表 肾小球IGFBP-1在2型DKD早期降低
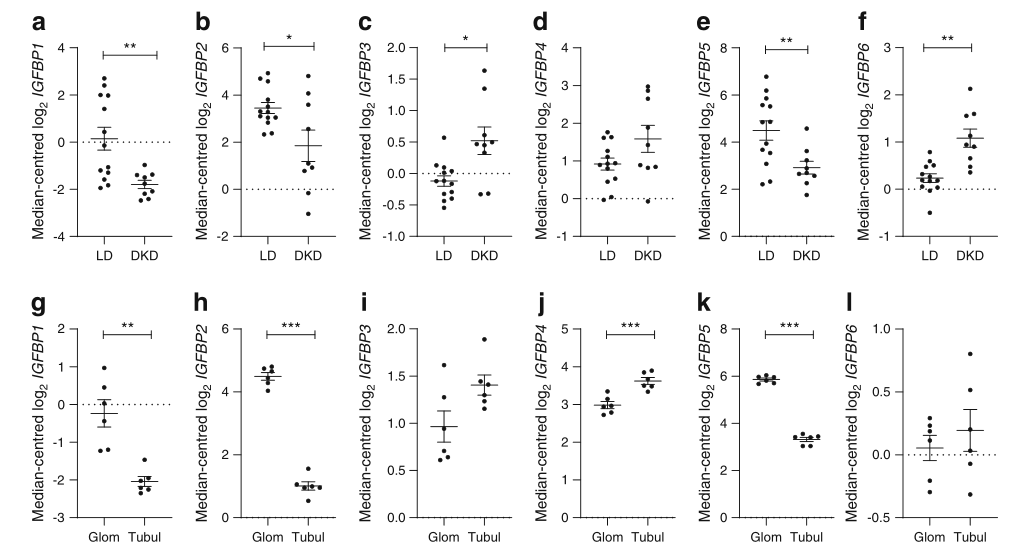
图1 在2型DKD中观察到肾小球IGFBP表达的变化。比较(A)IGFBP1的表达(以中位数为中心的log2)(q=0.02),(B)IGFBP2(q=0.18),(C)IGFBP3(q=0.04),(D)IGFBP4(q=0.41),(E)Igfbp5(q=0.0 4)DKD组(n=9)肾小球中1个nd(F)IGFBP6(q=0.09),与健康组(n=1 3)比较,*P<0.05,**p<0.01(G)IGFBP1(q=0.006),(H)IGFBP2(q=1.23×10−7),(I)IGFBP3(q=0.06),(J)IGFBP4(q=0.001),(K)IgFBP5(q=1.19×10−7)和nd(L)IGFBP6(q=0.46),每组6例,**p<0.0 1,*p<0.001,经Welch’sttest检验,q值用BenjiminHochberg法调整。LD,活体供体;肾小球,肾小管;肾小管间质
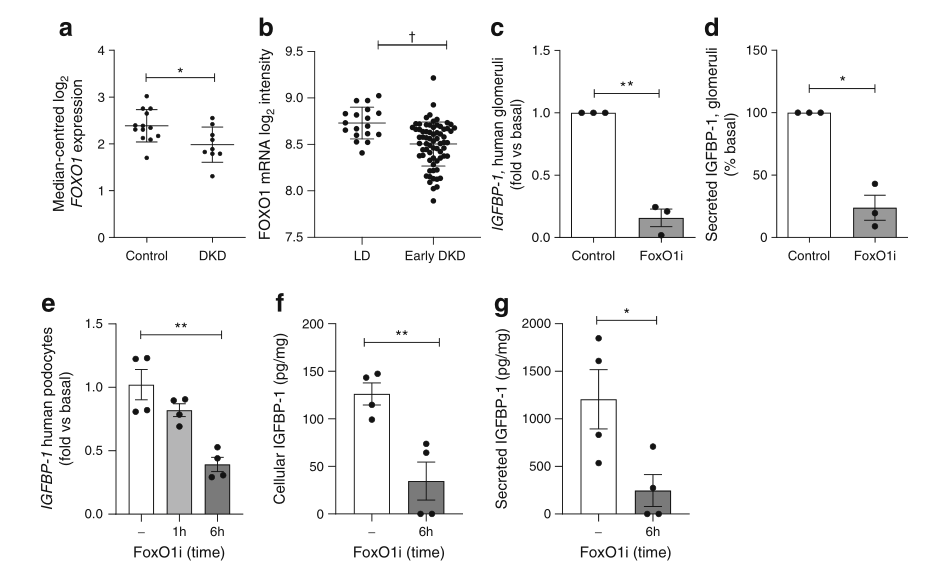
图2 IGFBP-1在人肾小球和足细胞中的表达受FoxO1调控。(A)Nephroseq:FOXO1 Woroniecka糖尿病Glom数据库中的表达,健康活体供者(n=1 3)vsDKD(n=9),*p=0.0 2,W e l c hsttest(qvalue=0.10)。(B)PIMA型2型糖尿病早期糖尿病组(早期DKD组,69例)与活体供者组(LD组,n=18)中FOXO1的表达(log2mRNA强度),†q=0.0003。(C)人离体肾小球IGFBP-1mRNA的Q-P-C R结果;(D)FoxO_1抑制(50 ng/ml AS1842856 FoxO_1抑制剂)10天后,肾小球培养液中IGFBP-1浓度的变化,n=3,P<0.0 5,**p<0.0 1,测试。(E)IGFBP-1mRNA表达的qPCR结果(n=4),**p<0.01,采用Tukey‘s多重比较检验。(F)足细胞裂解物中IGFBP-1水平归一化为总蛋白(n=4),**p=0.007。(G)FoxO1抑制6h后足细胞培养液中IGFBP-1浓度(50 ng/mlAS1842856)(n=4),*p=0.0 3,t检验,6h与基础值比较。FoxO1i,FoxO1抑制剂;qPCR,定量PCR
结论:本研究确认了IGFBP-1在足细胞功能调节中的新作用,并且在2型DKD早期,通过降低FoxO1活性,使得IGFBP-1的肾小球表达减少。因此,我们假设维持肾小球IGFBP-1水平的策略可能有利于在DKD早期维持足细胞功能。
原文出处:
Lay AC, Hale LJ, Stowell-Connolly H,et al,IGFBP-1 expression is reduced in human type 2 diabetic glomeruli and modulates β1-integrin/FAK signalling in human podocytes.Diabetologia 2021 Jul;64(7)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
32
#IGF#
58
#FAK#
46
#BET#
39
学习
54