JAMA Pediatr:脐带管理与早产儿不良预后
2021-03-15 MedSci原创 MedSci原创
与立即结扎脐带相比,延迟结扎脐带可降低早产儿死亡率,而延迟结扎和挤压脐带可降低早产儿脑室出血和红细胞输注风险
胎盘输血是指在胎儿出生后,立即将脐带血通过胎盘传递到新生儿体内,以增加新生儿的血容量。有研究认为,胎盘输血额外增加的血容量与降低早产儿不良事件风险相关。在许多医疗机构中,早产儿延迟结扎脐带(DCC,≥30s)是早产儿临床管理的重要部分。

近日研究人员开展系统综述及荟萃研究,比较了几种常见的新生儿脐带护理手段:立即结扎脐带(ICC)、延迟结扎脐带(DCC)与挤压脐带(UCM)对早产儿预后的影响。
研究人员收集了截至2020年9月,收录于PubMed、Embase、CINAHL和Cochrane的相关研究报道,涉及不同早产儿脐带管理方式对预后影响的研究。研究的主要终点为早产儿死亡,次要终点为脑室出血、严重脑室出血、需要红细胞输注以及其他新生儿疾病。
本次荟萃研究纳入56个临床研究,包含6852名早产儿,与ICC相比,DCC组早产儿的死亡率(22个研究,3083名患儿,7.6% vs 5.0%,OR=0.64)、脑室出血风险(25个研究,3316名患儿,17.8% vs 15.4%,OR=0.73)以及红细胞输注(18个研究,2904名患儿,46.9% vs 38.3%,OR=0.48)风险较低。与ICC相比,UCM组早产儿的脑室出血风险(10个研究,645名患儿,22.5% vs 16.2%,OR=0.58)以及红细胞输注(9个研究,688名患儿,47.3% vs 32.3%,OR=0.36)风险较低。组间其他终点事件差异不显著,DCC与UCM组患儿预后差异不显著。
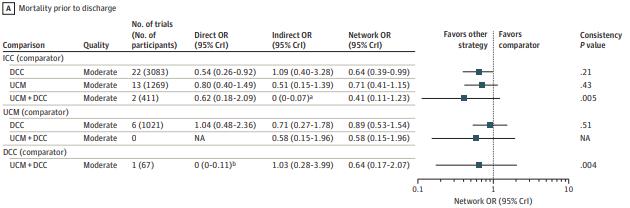
研究认为,与立即结扎脐带相比,延迟结扎脐带可降低早产儿死亡率,而延迟结扎和挤压脐带可降低早产儿脑室出血和红细胞输注风险。
原始出处:
Bonny Jasani et al. Association of Umbilical Cord Management Strategies With Outcomes of Preterm Infants A Systematic Review and Network Meta-analysis. JAMA Pediatr. March 8, 2021.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
41
#DIA#
41
#JAMA#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
105
学习
79
#不良预后#
0
#脐带#
44
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
60