European Radiology:加强骨水泥成形术在治疗盆腔肿瘤病变和盆腔外伤性骨折方面的价值
2022-08-23 shaosai MedSci原创
众所周知,无论是肿瘤性的还是创伤性的盆腔病变都可能是极其痛苦的,并严重损害患者的生活质量。骨转移是晚期癌症患者的最常见的发现。大约90%需要手术干预的骨折发生在股骨、肱骨或髋关节周围的骨区。强化骨水泥
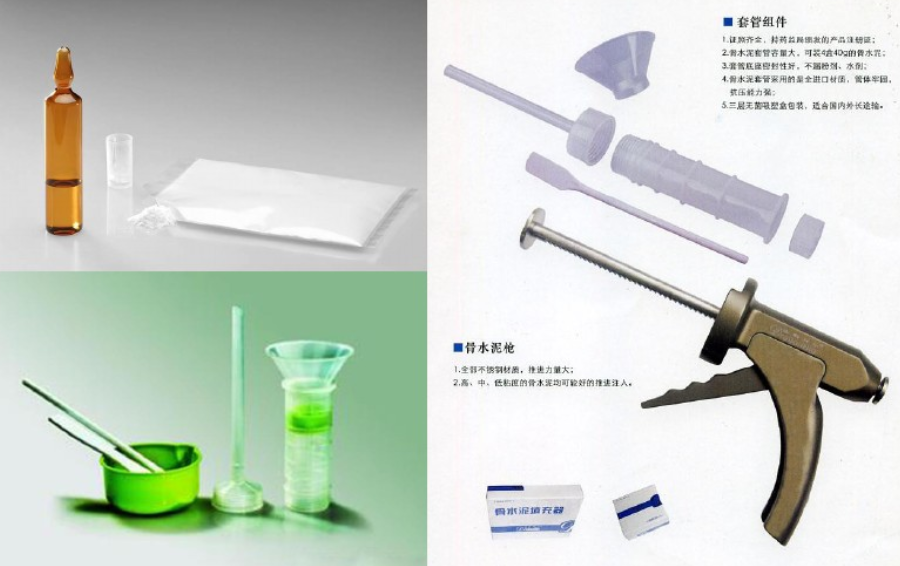
众所周知,无论是肿瘤性的还是创伤性的盆腔病变都可能是极其痛苦的,并严重损害患者的生活质量。骨转移是晚期癌症患者的最常见的发现。大约90%需要手术干预的骨折发生在股骨、肱骨或髋关节周围的骨区。强化骨水泥成形术(RC)是一种微创技术,结合使用专用针,通过骨针经皮插入骨病灶注射骨水泥,在治疗股骨近端骨转移方面显示出其极高的临床有效性。
近日,发表在European Radiology杂志的一项研究评估了RC对于治疗疼痛性盆腔病变和盆腔骨折的有效性,为进一步提高该类患者的治疗效果及临床预后提供了参考依据。

所有在本机构2013年11月-2017年10月期间进行了骨盆骨RC的肿瘤性病变或骨盆骨折的患者都被纳入本项研究中。所有药物治疗失败的患者、不适合手术的患者以及不稳定的溶骨性病变患者都有进行RC的指征。临床结果是通过术后1个月和6个月的随访进行评估的。主要终点是通过视觉模拟量表(VAS)测量的局部疼痛缓解进行评估。
在研究期间,有22名患者(18名女性,4名男性;平均年龄为65.4±13.3岁[范围38-80])因疼痛和不稳定的骨盆病变而接受了RC治疗。在这22名患者中,有8名患者出现了不稳定的骨盆骨折(3名患者为髂嵴骨折,3名为骶骨骨折,其余2名为髋关节周围骨折)。没有手术相关的并发症记录。所有患者在1个月时都有明显的疼痛缓解和功能改善。一名患者(4.5%)由于局部肿瘤的发展而发生了二次骨折。

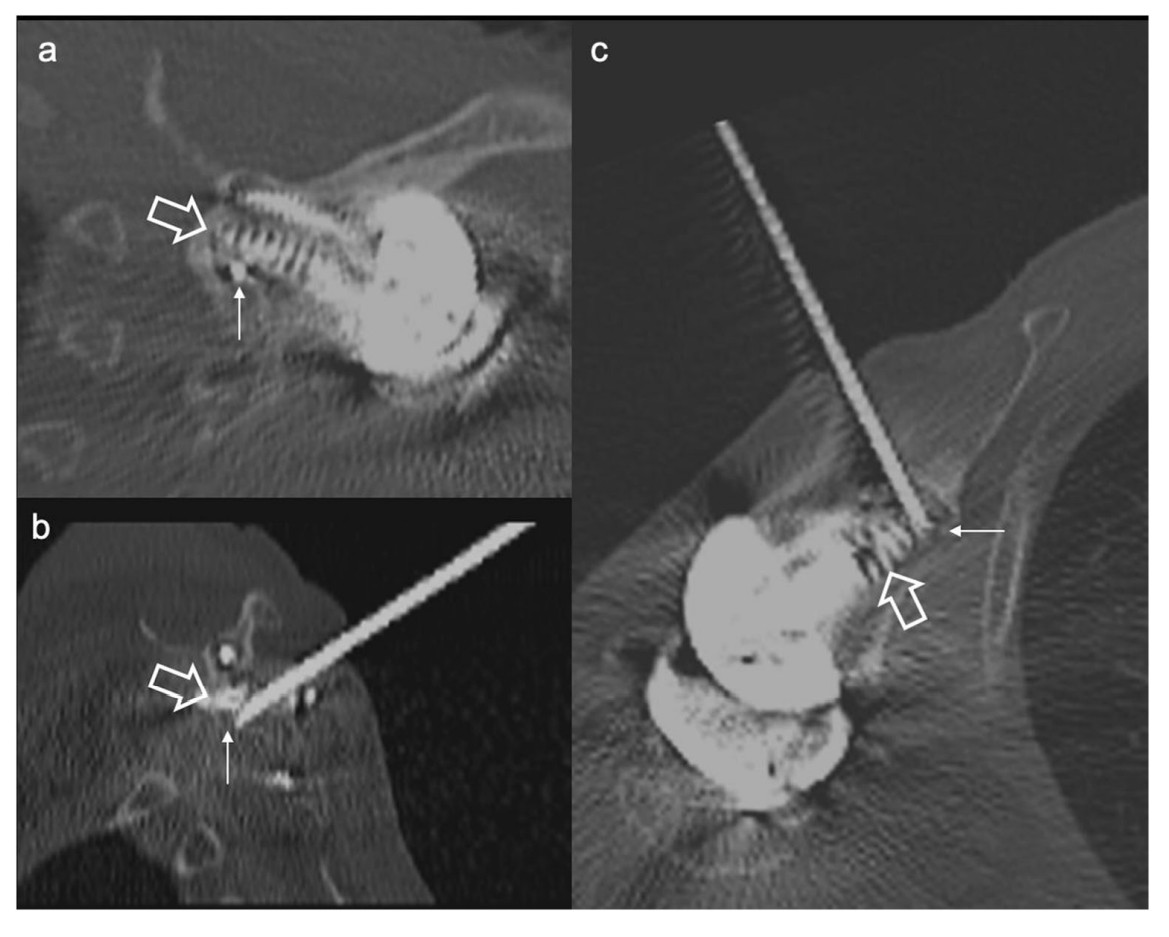
图 一名74岁的女性在滑雪时摔倒后出现右髋臼骨折。A 平扫CT扫描图像显示无移位的右髋臼骨折(箭头)。B 术中前后向(AP)透视显示针头穿过骨折处的位置(箭头)。C 注入骨水泥后的对照X光片(AP),显示骨水泥在钉子周围的分布令人满意。该患者在随访期间没有发生二次骨折
本研究表明,强化骨水泥成形术是一种原始的微创技术,通过对已完成或即将发生的盆骨病理性骨折进行有效的骨稳定,有助于缓解疼痛、提高患者的生活质量,可以被常规纳入骨不全骨折以及疼痛性转移性骨病的治疗方案范围。
原文出处:
Amira Al Raaisi,Kévin Premat,Evelyne Cormier,et al.Reinforced cementoplasty for pelvic tumour lesions and pelvic traumatic fractures: preliminary experience.DOI:10.1007/s00330-022-08742-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#成形术#
43
#PE#
28
#外伤性#
46
#骨水泥#
40