Crit Care:脓毒症/脓毒性休克患者高氧血症与死亡率降低相关
2022-01-10 MedSci原创 MedSci原创
PaO2高于100mmHg与重症术后脓毒症/感染性休克患者的90天死亡率、ICU停留时间和插管时间相关。
尽管人们对限制ICU患者吸氧的治疗策略越来越感兴趣,但没有研究将保守吸氧与标准吸氧在伴有脓毒症/脓毒性休克术后患者中进行比较,尽管有迹象表明它可能会改善患者预后。已经有研究证明,动脉血中的高氧分压(PaO2)可降低大手术患者的手术伤口感染率和死亡率。

近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,该研究旨在评估PaO2是否与成年脓毒症/感染性休克患者大手术后的死亡风险相关。
研究人员对一项前瞻性观察研究进行了二次分析,该研究纳入了454名接受大手术并入住ICU的患者。根据在脓毒症/感染性休克发作当天是否伴有高氧血症,将患者分为两组。高氧血症定义为PaO2>100mmHg(n=216),或PaO2≤100mmHg(n=238)。该研究的主要终点是脓毒症诊断后的90天死亡率,次要终点是ICU住院时间和拔管时间。
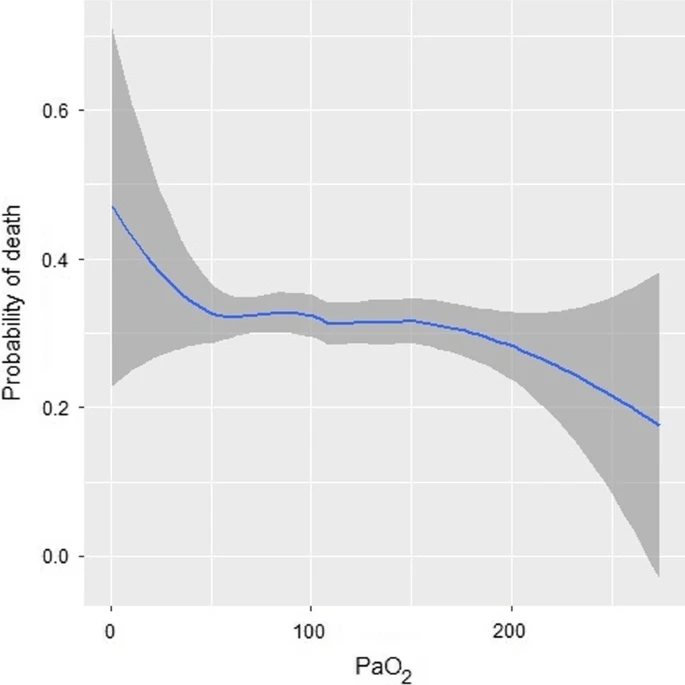
在PaO2≤100mmHg的患者中,研究人员发现机械通气时间延长(2[8] vs 1[4]天,p<0.001),ICU停留时间更长(8[13] vs 5[9]天,p<0.001),通过SOFA评分评估的器官功能障碍严重程度较高(9[3] vs 7[5],p<0.001),感染性休克的患病率较高(200/238,84.0% vs 145/216)67.1%,p<0.001)以及90天死亡率更高(37.0%[88] vs 25.5%[55],p=0.008)。在多变量分析中,高氧血症与较高的90天生存率相关(OR为0.61,95%CI为0.39-0.95,p=0.029),而与年龄、慢性肾功能衰竭、降钙素原水平和APACHEII评分>19无关。当排除研究纳入时患有严重低氧血症的患者时,这些结果也得到了证实。
由此可见,PaO2高于100mmHg与重症术后脓毒症/感染性休克患者的90天死亡率、ICU停留时间和插管时间相关。
原始出处:
Marta Martín-Fernández,et al.Hyperoxemia in postsurgical sepsis/septic shock patients is associated with reduced mortality.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03875-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脓毒性#
51
#高氧血症#
40
学习到了
52
#脓毒性休克#
43