NEJM:婴儿出现生长抑制:IGF2基因突变是真凶!
2015-07-10 姜英浩 MedSci原创
胰岛素样生长因子2(IGF2),又称生长调节素A,是一个单链多肽分子。IGF2是一个在细胞增殖、分化、程序性死亡和转化中具有重要的作用的细胞因子,对个体生长、发育具有重要作用,人类的许多疾病的发生发展都与该基因的异常有关
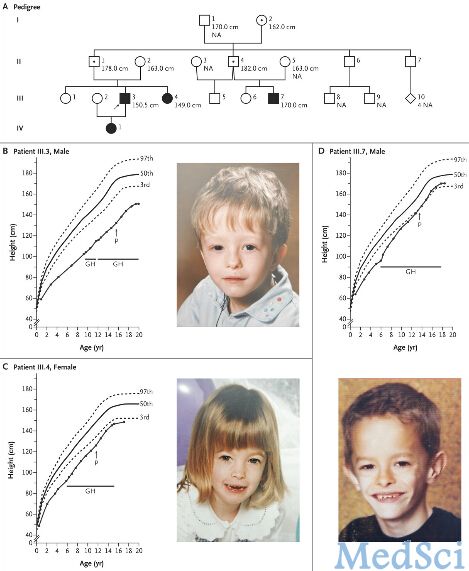
胰岛素样生长因子2(IGF2),又称生长调节素A,是一个单链多肽分子。IGF2是一个在细胞增殖、分化、程序性死亡和转化中具有重要的作用的细胞因子,对个体生长、发育具有重要作用,人类的许多疾病的发生发展都与该基因的异常有关。在2015年7月8日新英格兰医学杂志(New England Journal of Medicine)上在线发表的一篇论文表示,IGF2的一种突变形式——(c.191C→A, p.Ser64Ter)会使得从父方遗传到该突变的婴儿在出生前及出生后的生长都受到严重的抑制。
该研究结果由德国亚琛Rhine-Westphalia科技研究所的Matthias Begemann博士及其研究团队发布。他们在患者家庭中几代人内发现了IGF2基因突变会造成病理性变化的证据。考虑到以往有研究发现IGF1与IGF1R在子宫内及出生后胎儿生长抑制中发挥的作用,该研究团队将目光转向IGF2基因,及其编码的胰岛素样生长因子II,期望发现其产生的功能和影响。
本研究募集了4位被确诊患有严重生长抑制的家庭成员。研究人员发现仅有当从父方遗传获得该突变时,患者才能产生该疾病表型,此结果与母方IGF2的基因印记结果一致。患病的家庭成员出现了严重的生长抑制症状,该结果预示着IGF2能够同时影响胎儿出生前及出生后的生长状况。患病的家庭成员同时也会出现体型体态异常的症状,该现象也与既往报道的IGF2缺陷参与了Silver-Russell syndrome(一种使儿童身体畸形的症状)的发生发展一致。
该研究论文的作者提出:“在出现生长抑制的患者中发现了IGF2基因的突变表明,IGF2不仅仅调控了子宫内生长发育,同时也参与了出生后生长过程,具有功能的多样性。本研究结果提示利用重组人生长激素进行治疗具有一定的潜力和希望。”
原文出处:
Matthias Begemann, Birgit Zirn, Gijs Santen, et al. Paternally Inherited IGF2 Mutation and Growth Restriction. The New England Journal of Medicine. 2015. 7.8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错,赞一个
139
这篇文章有一定深度
130
是一篇不错的文章
124
值得进一步关注
114
#IGF#
35
看看
152
!
76
?
55
?
57
?
72