Nat Commun:科学家发现再生血管的关键,为心血管病治疗带来新曙光
2017-11-23 佚名 medicalxpress
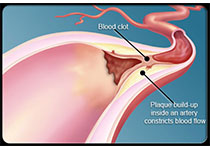
由Sanford Burnham Prebys医学发现研究所(SBP)的研究人员领导的一项新研究确定了一个信号通路,该通路对血管生成以及来自已有血管的新血管的生长是必不可少的。 “自然通讯”杂志发表的研究结果可能改善目前的策略,改善缺血组织的血流量,如动脉粥样硬化和糖尿病相关的外周血管疾病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










如果vegf和rras都是通过激活akt发挥作用,那么为何得到不同结果?
61
#科学家发现#
33
#COMMUN#
35
#血管病#
28
#Nat#
28
#曙光#
34
学习了谢谢分享!!
65