贫血是亟需关注的一类疾病——天津医科大学总医院邵宗鸿教授谈贫血诊治现状
2018-03-14 佚名 中华医学信息导报
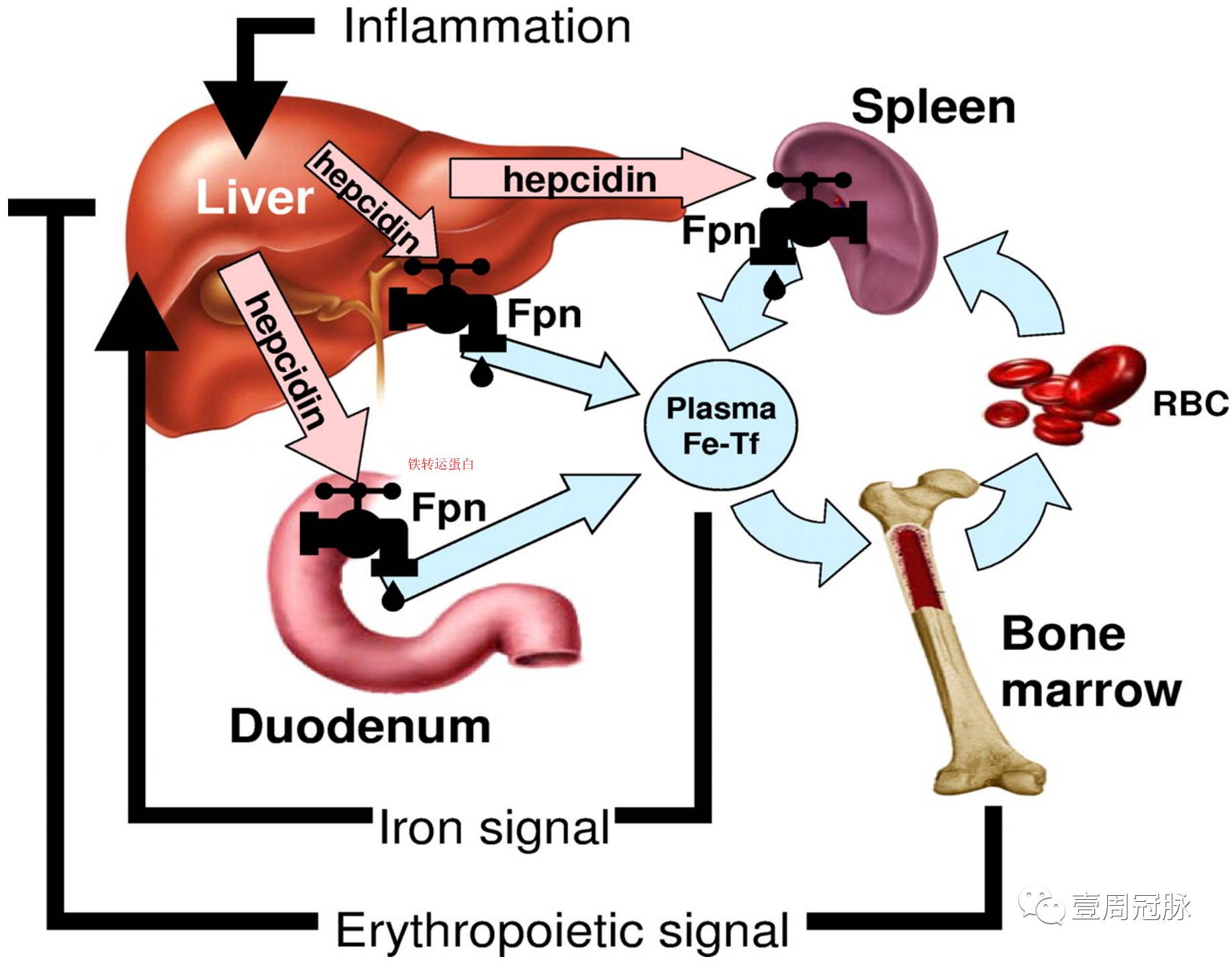
2013年发布的《2010年全球疾病负担评估》报告中指出,1990~2010年187个国家的贫血患病率为32.9%,伤残调整生命年高达683.6万年。研究表明,全球约24.8%的人口患有贫血,中国的贫血患病率约为20.1%,其中超半数是因缺铁所致,缺铁性贫血也是许多严重疾病的常见并发症。慢性肾病患者、育龄女性、妊娠人群和发育中的儿童是缺铁性贫血的高危人群。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#医科大学#
48
#总医院#
32
#诊治现状#
48
好
62
缺铁性贫血这么多
67
学习学习学习
77
谢谢分享有点意思
2
学习谢谢分享
59
学习了受益匪浅
31
好文.值得点赞!认真学习.应用于实践!谢谢分享给广大同好!
25