CNS Drugs:SSRIs在改善脑卒中后功能结局上有何作用?
2018-10-27 吴星 环球医学网
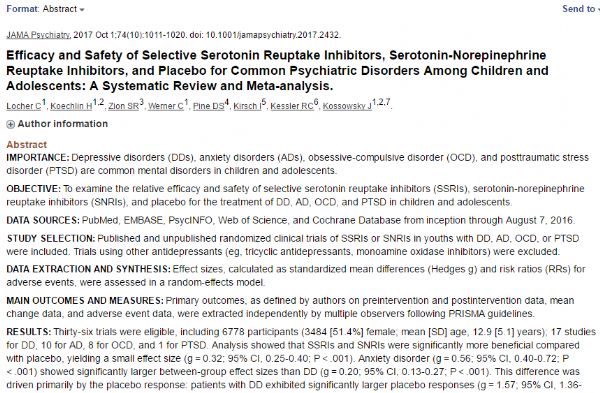
2018年10月,发表于《CNS Drugs》上的一项研究,考察了选择性5-羟色胺再摄取抑制剂(SSRIs)改善脑卒中后功能结局方面的潜在作用。
过去几十年来,急性卒中治疗取得的巨大进展极大地改变了卒中后的生活。然而,静脉溶栓治疗和血管内血栓切除术受到相对狭窄的时间窗或治疗禁忌证的限制。此外,纵然身体问题或许几乎消失,使用急性再灌注疗法的患者由于潜在脑梗死还存在认知和情感方面的并发症。
总之,卒中仍然是全世界成人失能和死亡的一个常见原因。需要提供更多最好在急性期后也可行的治疗方案,以改善康复。尽管多种药物和治疗方式促进卒中后康复的潜力得以研究,但是,没有明确可以增强康复进程的治疗。一类有希望的治疗药物是SSRIs,这是一类常用的具有神经再生特性的抗抑郁药物。
这篇研究回顾了SSRIs作为卒中恢复潜在增强剂的证据,并讨论了所报告影响的潜在机制以及对卒中后患者管理的影响,包括潜在的不良事件和药物-药物相互作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CNS#
41
#卒中后#
36
#Drug#
32
#drugs#
32
#功能结局#
33
#SSRI#
42
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
44